November 1, 2015
◆
Volume 92, Number 9 www.aafp.org/afp American Family Physician 807
Cognitive behavior therapy (CBT) is a time-limited, goal-oriented psychotherapy that has been extensively researched
and has benefits in a number of psychiatric disorders, including anxiety, depression, posttraumatic stress disorder,
attention-deficit/hyperactivity disorder, autism, obsessive-compulsive and tic disorders, personality disorders, eating
disorders, and insomnia. CBT uses targeted strategies to help patients adopt more adaptive patterns of thinking and
behaving, which leads to positive changes in emotions and decreased functional impairments. Strategies include iden-
tifying and challenging problematic thoughts and beliefs, scheduling pleasant activities to increase environmental
reinforcement, and extended exposure to unpleasant thoughts, situations, or physiologic sensations to decrease avoid-
ance and arousal associated with anxiety-eliciting stimuli. CBT can be helpful in the treatment of posttraumatic stress
disorder by emphasizing safety, trust, control, esteem, and intimacy. Prolonged exposure therapy is a CBT technique
that includes a variety of strategies, such as repeated recounting of the trauma and exposure to feared real-world situ-
ations. For attention-deficit/hyperactivity disorder, CBT focuses on establishing structures and routines, and clear
rules and expectations within the home and classroom. Early intensive behavioral interventions should be initiated in
children with autism before three years of age; therapy consists of 12 to 40 hours of intensive treatment per week, for at
least one year. In many disorders, CBT can be used alone or in combination with medications. However, CBT requires
a significant commitment from patients. Family physicians are well suited to provide collaborative care for patients
with psychiatric disorders, in concert with cognitive behavior therapists. (Am Fam Physician. 2015;92(9):807-812.
Copyright © 2015 American Academy of Family Physicians.)
Common Questions About Cognitive
Behavior Therapy for Psychiatric Disorders
SCOTT F. COFFEY, PhD, and ANNE N. BANDUCCI, PhD, University of Mississippi Medical Center, Jackson, Mississippi
CHRISTINE VINCI, PhD, University of Texas M.D. Anderson Cancer Center, Houston, Texas
C
ognitive behavior therapy (CBT)
is a group of time-limited, goal-
oriented psychotherapies that have
been extensively researched for the
treatment of psychiatric disorders. CBT tar-
gets changes in symptoms of psychiatric dis-
orders to reduce functional impairments and
improve patients’ overall quality of life. This
article aims to provide a concise overview of
CBT, including the types of disorders it can
treat, how it can be combined with pharma-
cotherapy, and how family physicians can use
CBT principles in their practice.
Which Patients Benefit from CBT?
CBT is effective for the treatment of anxiety,
depression, posttraumatic stress disorder
(PTSD), attention-deficit/hyperactivity dis-
order (ADHD), autism, obsessive-compulsive
and tic disorders, personality disorders, eat-
ing disorders, and insomnia. CBT-based
treatments for specific disorders are avail-
able at http://www.abct.org/Information/
?m=mInformation&fa=FactSheets.
EVIDENCE SUMMARY
CBT effectively targets symptoms of anxiety,
1-4
depression,
5-7
PTSD,
8,9
ADHD,
10,11
autism,
12,13
obsessive-compulsive and tic disorders,
14
personality disorders,
15,16
eating disorders,
17
and insomnia
18
in children, adolescents, and
adults. Numerous meta-analyses and reviews
have demonstrated that CBT reduces psychi-
atric symptoms and functional impairments,
and improves quality of life.
1-18
The Ameri-
can Psychological Association lists CBT as an
effective treatment for numerous disorders.
19
Moreover, CBT has been shown to be as effec-
tive as or more effective than medications
for depression, anxiety, and trauma-related
disorders,
5,9,20-29
and it is a useful adjunctive
therapy for disorders such as ADHD, schizo-
phrenia, and bipolar disorder.
10-12,22,23
How Does CBT Work?
According to the cognitive behavioral model,
psychopathology occurs because of problem-
atic patterns in thinking and behavior that
lead to difficult emotions and functional
CME
This clinical content
conforms to AAFP criteria
for continuing medical edu-
cation (CME). See CME Quiz
Questions on page 764.
Author disclosure: No rel-
evant financial affiliations.
▲
Patient information:
A handout on this topic,
written by the authors of
this article, is available at
http://www.aafp.org/afp/
2015/1101/p807-s1.html
Downloaded from the American Family Physician website at www.aafp.org/afp. Copyright © 2015 American Academy of Family Physicians. For the private, noncom-
mercial use of one individual user of the website. All other rights reserved. Contact copyrights@aafp.org for copyright questions and/or permission requests.
Cognitive Behavior Therapy
808 American Family Physician www.aafp.org/afp Volume 92, Number 9
◆
November 1, 2015
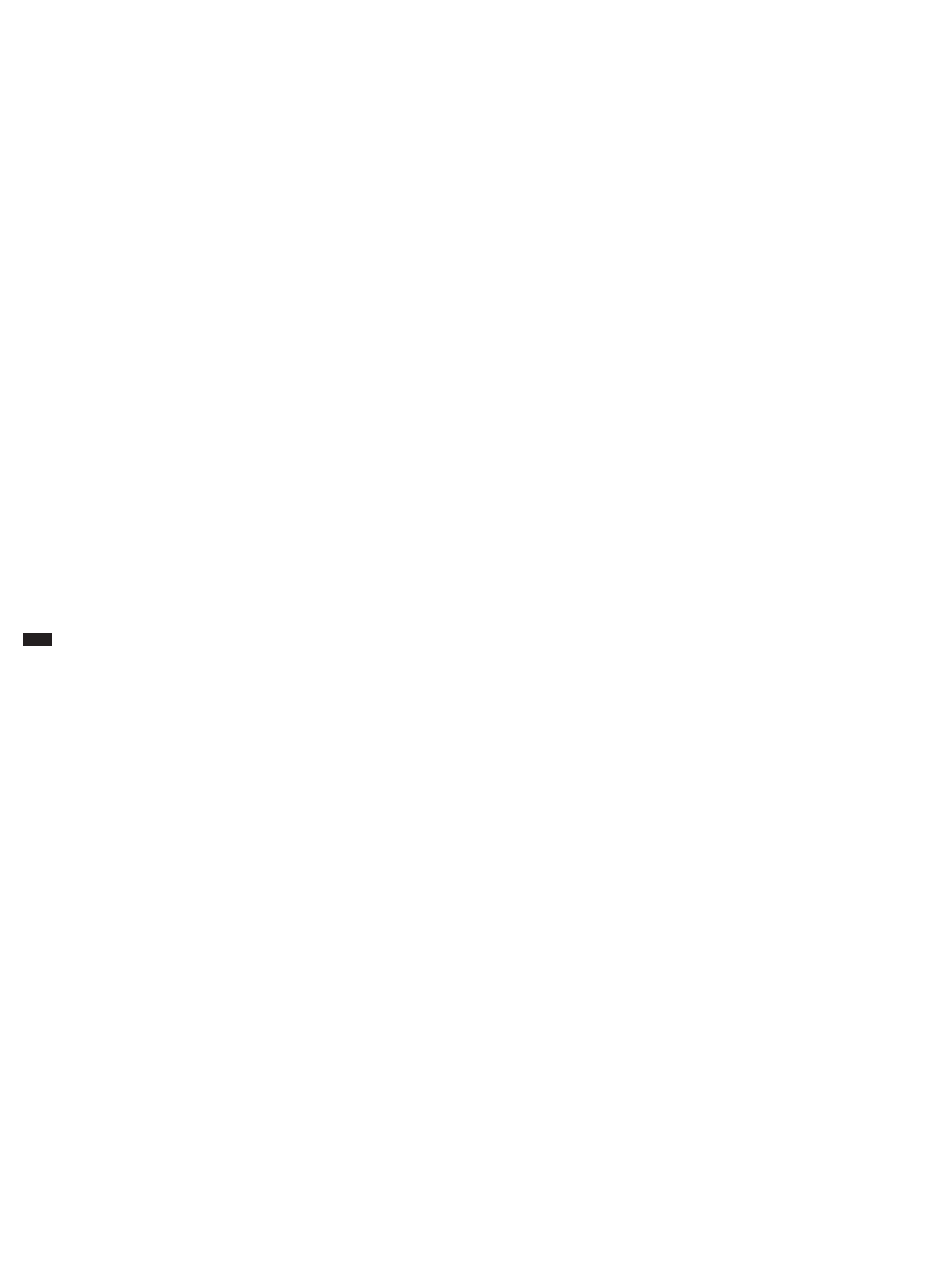
impairments (Figure 1). The aim of CBT is to help patients
adopt more adaptive patterns of thinking and behavior
to improve function and quality of life. Treatment goals
are selected collaboratively with patients to determine
whether progress is being made. CBT involves three core
strategies applied alone or in combination, depending
on the patients’ needs: (1) identifying and challenging
problematic thoughts and beliefs, with the goal of help-
ing patients develop more realistic and adaptive thoughts
and beliefs, (2) scheduling pleasant activities to increase
environmental reinforcement, and (3) extended exposure
to unpleasant thoughts, situations, or physiologic sensa-
tions to decrease avoidance and arousal associated with
anxiety-eliciting stimuli.
30
EVIDENCE SUMMARY
Research demonstrates that problematic patterns of
thinking and behavior underlie most forms of psychopa-
thology.
30
Behavioral change has been shown to lead to
cognitive changes, and vice versa; these changes lead to
reductions in psychopathology.
5,6
How Does CBT Improve Depression?
A cognitive behavior therapist whose patient
feels sad and hopeless might choose to tar-
get the patient’s maladaptive thoughts (“I
cannot connect with anyone.”) or behaviors
(isolating and watching television). Targeting
changes in either domain leads to changes in
the other and in the patient’s emotions.
5,6
For
example, the therapist might challenge the
patient’s thoughts by eliciting examples of
occasions when the patient was able to posi-
tively engage with others. This could cause
the patient to feel less hopeless as he or she
realizes that the thought was not accurate,
and to call a friend to reconnect. Alterna-
tively, the therapist could attempt to change
the maladaptive behaviors by helping the
patient schedule pleasant activities consistent
with his or her values (calling a friend). This
reconnection could boost the patient’s mood
and change the belief that he or she will
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Clinical recommendation
Evidence
rating References
CBT is an effective treatment for mild to moderate depression, anxiety disorders, posttraumatic
stress disorder, obsessive-compulsive and tic disorders, autism, eating disorders, personality
disorders, insomnia, and attention-deficit/hyperactivity disorder.
A 1-18, 34-37
Psychiatric medications are the primary treatment for schizophrenia and bipolar disorder, but CBT
provides additional benefits.
B 22, 23
For many psychiatric conditions, CBT provides similar outcomes or additional benefits compared
with psychiatric medications alone.
A 5, 9-11, 18, 20,
22, 24-27
Benzodiazepine use should be avoided in patients who are receiving CBT because it can interfere
with exposure therapy.
C 38-41
CBT = cognitive behavior therapy.
A = consistent, good-quality patient-oriented evidence; B = inconsistent or limited-quality patient-oriented evidence; C = consensus, disease-oriented
evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, go to http://www.aafp.org/afpsort.
Figure 1. The cognitive behavioral model illustrates problematic pat-
terns in thoughts and behaviors that lead to emotional difficulties
and functional impairments.
Cognitive Behavioral Model
Thoughts (e.g., “I cannot
connect with anyone and
will always be alone.”)
Behaviors (e.g.,
isolating, watching
television, overeating,
using substances)
Feelings (e.g., sadness,
loneliness, angry at self)
Cognitive Behavior Therapy
November 1, 2015
◆
Volume 92, Number 9 www.aafp.org/afp American Family Physician 809
always be alone. Although these examples
misrepresent the amount of therapeutic work
needed to change entrenched patterns of
thoughts and behaviors, they give a sense of
what the therapeutic process might involve.
EVIDENCE SUMMARY
CBT can be used to reduce symptoms
of depression, with or without medica-
tion.
5-7,20-29,31-33
Although treatment guidelines
from the American Psychiatric Association
suggest that medication should be used as a
first-line treatment for depression, CBT should
also be considered. Evidence has shown that
CBT and paroxetine (Paxil) produce equivalent outcomes
in patients with severe depression.
34
Thus, family physi-
cians must use their clinical judgment in determining
which treatments to suggest for their patients.
How Does CBT Improve Anxiety and Trauma-
Related Disorders?
Similar to the example above, therapists who are treating
patients with anxiety and trauma-related disorders chal-
lenge problematic patterns of thoughts or behaviors. A
more thorough description of CBT for PTSD is provided
here as an example.
Evidence-based therapies for PTSD in adults include
cognitive processing therapy and prolonged expo-
sure therapy, whereas trauma-focused CBT is used in
younger patients. Cognitive processing therapy includes
psychoeducation about PTSD and focuses on challeng-
ing maladaptive thoughts and beliefs about safety, trust,
control, esteem, and intimacy.
35
Prolonged exposure
therapy includes psychoeducation about PTSD, breath-
ing retraining to decrease arousal, repeated recounting
of the trauma to teach patients that the memories are not
dangerous and do not need to be avoided, and in vivo
exposure to feared real-world situations.
8,9
In younger
patients, trauma-focused CBT includes components
similar to those for prolonged exposure and cognitive
processing therapies, but also includes parallel and joint
parental sessions.
36
EVIDENCE SUMMARY
CBT techniques for the treatment of PTSD can be
applied across all anxiety and trauma-related disorders
in children, adolescents, and adults.
1-3,35-37
Is CBT Different When Used in Children vs. Adults?
Parental involvement in therapy is necessary when chil-
dren receive CBT. Parents can ensure that their child
engages in behavioral exercises between therapy sessions
(e.g., in vivo exposures, pleasant activities), can change
the child’s environment to promote more effective
behaviors, and can help the child target changes in mal-
adaptive thoughts. In general, CBT for children focuses
more on behavior changes and less on cognitive changes.
Behavioral techniques used for children with ADHD and
autism are described below.
ADHD
A recent review showed that behavioral parent training,
behavioral classroom management, and behavioral peer
interventions are well-established treatments for ADHD.
11
Behavioral parent training and behavioral classroom
management focus on strategies implemented by adults
to help children with ADHD function more effectively,
including creating structure and routines, setting clear
rules and expectations, using effective commands, and
rewarding or punishing the child based on his or her com-
pliance. These techniques help reduce behavioral prob-
lems experienced by children with ADHD and decrease
the need for polypharmacy to manage symptoms.
11
AUTISM
Early intensive behavioral interventions are the only
evidence-based treatment that confers significant bene-
fits in children with autism.
12
These interventions should
be initiated before three years of age and often consist
of 12 to 40 hours of intensive treatment per week, for at
least one year. Parents and therapists engage in intensive
exercises focused on reinforcing and rewarding adaptive
behaviors. Behavioral treatments for autism produce sig-
nificant improvements in IQ and adaptive behaviors.
13
EVIDENCE SUMMARY
Behavioral therapy is the only effective treatment for
autism
12
and is an important adjunctive treatment for
BEST PRACTICES IN PSYCHIATRY: RECOMMENDATIONS
FROM THE CHOOSING WISELY CAMPAIGN
Recommendation Sponsoring organization
Avoid use of hypnotics as primary therapy for
chronic insomnia in adults; instead, offer
cognitive behavior therapy, and reserve
medication for adjunctive treatment when
necessary.
American Academy of
Sleep Medicine
Do not prescribe medication to treat childhood
insomnia, which usually arises from parent-
child interactions and responds to behavioral
intervention.
American Academy of
Sleep Medicine
Source: For more information on the Choosing Wisely Campaign, see http://
www.choosingwisely.org. For supporting citations and to search Choosing
Wisely recommendations relevant to primary care, see http://www.aafp.org/afp/
recommendations/search.htm.

Cognitive Behavior Therapy
810 American Family Physician www.aafp.org/afp Volume 92, Number 9
◆
November 1, 2015
ADHD.
10,11
In addition, CBT provides substantial ben-
efits for children with depression or anxiety.
3,7
Is CBT Effective for Other Disorders?
CBT has been examined and tested across a wide range
of psychiatric disorders. In addition, it has been exam-
ined as an adjunctive treatment for medical problems in
which behavior change could enhance outcomes.
EVIDENCE SUMMARY
Although a thorough discussion of the effectiveness of
CBT for all psychiatric disorders is beyond the scope of
this article, it has been shown to have significant benefits
for patients with insomnia,
18
psychosis,
23
bipolar disor-
der,
22
eating disorders,
17
and personality disorders.
15,16
Family physicians are encouraged to seek adjunctive
CBT for patients diagnosed with these disorders.
When Can CBT Be Combined with Medications?
CBT can be used alone or in combination with medica-
tions for a variety of psychiatric disorders. Medications
can be used to stabilize patients and promote recov-
ery, whereas CBT can be used to encourage long-term
changes in thoughts and behaviors.
EVIDENCE SUMMARY
CBT generally produces equivalent outcomes or provides
additional benefits compared with the use of psychiatric
medications alone.
5,9,12,20-23,26,34
Moreover, CBT is often
more cost-effective, has more enduring effects,
9,21-23,27,28
and lacks the adverse effects associated with many psy-
chiatric medications. The effects of CBT are reduced in
patients who are receiving benzodiazepines
38-40
; there-
fore, these medications should be avoided in patients
with anxiety and trauma-related disorders. Although a
combination of CBT and benzodiazepines may initially
seem beneficial (e.g., reduced arousal, improved sleep),
this approach may actually limit the gains made with
CBT (e.g., patients may not be able to engage in exposure
exercises when arousal is reduced as a result of medica-
tion use).
38,41
What Are the Potential Limitations of CBT?
CBT is most effective when patients complete therapeu-
tic exercises outside of the treatment session; therefore,
it requires a significant commitment from patients.
Some of the therapeutic strategies may involve anxiety-
eliciting stimuli, which can be distressing—although
short-lived—for some patients. The structured nature of
CBT is not a good fit for patients who are seeking insight
into the underlying causes of their distress. Lastly, CBT is
not a substitute for pharmacotherapy for some disorders.
For example, CBT should be considered an adjunctive
treatment in the management of bipolar disorder, psy-
chotic disorders, and depression with psychotic features.
How Can Family Physicians Integrate CBT
into Practice and Provide Referrals to Effective
Therapists?
When discussing psychiatric disorders with patients,
family physicians are well suited to help patients decide
which services to seek. In addition to asking about
patients’ personal and family histories of psychiatric
disorders, family physicians can help patients identify
thoughts and behaviors that are contributing to their
problems. For example, avoidance behaviors (e.g., avoid-
ing crowded stores, avoiding interacting with the oppo-
site sex) help maintain anxiety disorders and PTSD.
Family physicians can encourage patients to face safe
stimuli and, if possible, seek safe fear-eliciting stimuli.
For patients with depressive symptoms, encouraging
engagement in a daily pleasant activity is helpful.
32
Family physicians are on the front line when it comes to
treatments for psychiatric disorders and can be influential
when recommending treatments to their patients. Build-
ing a collaborative relationship with community-based
behavior therapists enables family physicians to provide
comprehensive care. Table 1 provides resources for CBT,
including websites for locating therapists and informa-
tion to help patients select a therapist. For patients who
are already engaged in therapy, family physicians can
help determine whether they would benefit from CBT,
especially if the alternative is a potentially longer-term,
less cost-effective form of psychotherapy. Table 2 lists key
features of CBT that physicians can incorporate into dis-
cussions to optimize their patients’ care.
Table 1. Cognitive Behavior Therapy Resources
for Family Physicians
Academy of Cognitive Therapy – Therapist locator
http://www.academyofct.org
American Psychological Association – Therapist locator
http://locator.apa.org/
Association for Behavioral and Cognitive Therapies
http://www.abct.org/Information/?m=mInformation&
fa=FactSheets, http://www.abct.org/information/?m=
mInformation&fa=fs_GUIDELINES_CHOOSING, and
http://www.abctcentral.org/xFAT/
Psychology Today – Therapist locator
https://therapists.psychologytoday.com/rms/prof_search.php
Cognitive Behavior Therapy
November 1, 2015
◆
Volume 92, Number 9 www.aafp.org/afp American Family Physician 811
Data Sources: A PsycINFO search was completed using the key terms
cognitive behavioral therapy, cognitive therapy, and behavior therapy.
The search included meta-analyses, randomized controlled trials, clinical
trials, and reviews. Search dates: October and November 2014. In addi-
tion, we used an evidence summary from Essential Evidence Plus.
The Authors
SCOTT F. COFFEY, PhD, is the director of the Division of Psychology and
vice chair for research in the Department of Psychiatry and Human Behav-
ior at the University of Mississippi Medical Center, Jackson.
ANNE N. BANDUCCI, PhD, is a postdoctoral research fellow at the National
Center for PTSD at the VA Palo Alto (Calif.) Health Care System. At the time
the article was written, she was a resident in the Department of Psychiatry
and Human Behavior at the University of Mississippi Medical Center.
CHRISTINE VINCI, PhD, is a postdoctoral research fellow in the Depart-
ment of Health Disparities Research at the University of Texas M.D. Ander-
son Cancer Center, Houston.
Address correspondence to Scott F. Coffey, PhD, University of Mis-
sissippi Medical Center, 2500 N. State St., Jackson, MS 39216 (e-mail:
scoffey@umc.edu). Reprints are not available from the authors.
REFERENCES
1. Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety
disorders: a meta-analysis of randomized placebo-controlled trials.
J Clin Psychiatry. 2008;69(4):621-632.
2. Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, Andersson G.
Psychological treatment of generalized anxiety disorder: a meta-analysis.
Clin Psychol Rev. 2014;34(2):130-140.
3. Reynolds S, Wilson C, Austin J, Hooper L. Effects of psychotherapy for
anxiety in children and adolescents: a meta-analytic review. Clin Psychol
Rev. 2012;32(4):251-262.
4. Sánchez-Meca J, Rosa-Alcázar AI, Marín-Martínez F, Gómez-Conesa A.
Psychological treatment of panic disorder with or without agorapho-
bia: a meta-analysis [published correction appears in Clin Psychol Rev.
2010;30 (6):815-817]. Clin Psychol Rev. 2010;30 (1):37-50.
5. Dobson KS, Hollon SD, Dimidjian S, et al. Randomized trial of behav-
ioral activation, cognitive therapy, and antidepressant medication in the
prevention of relapse and recurrence in major depression. J Consult Clin
Psychol. 2008;76(3):468-477.
6. Mazzucchelli T, Kane R, Rees C. Behavioral activation treatments for
depression in adults: a meta-analysis and review. Clin Psychol Sci Pract.
2009;16(4):383- 411.
7. Klein JB, Jacobs RH, Reinecke MA. Cognitive-behavioral therapy for
adolescent depression: a meta-analytic investigation of changes in
effect-size estimates. J Am Acad Child Adolesc Psychiatry. 20 07;4 6 (11) :
1403-1413.
8. Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-
analytic review of prolonged exposure for posttraumatic stress disorder.
Clin Psychol Rev. 2010;30 (6):635- 641.
9. Le QA, Doctor JN, Zoellner LA, Feeny NC. Cost-effectiveness of pro-
longed exposure therapy versus pharmacotherapy and treatment
choice in posttraumatic stress disorder (the Optimizing PTSD Treat-
ment Trial): a doubly randomized preference trial. J Clin Psychiatry.
2014;75(3):222-230.
10. Daley D, van der Oord S, Ferrin M, et al.; European ADHD Guidelines
Group. Behavioral interventions in attention-deficit/hyperactivity dis-
order: a meta-analysis of randomized controlled trials across multiple
outcome domains. J Am Acad Child Adolesc Psychiatry. 2014;53(8):835-
847, 847.e1-847.e5.
11. Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treat-
ments for children and adolescents with attention-deficit/hyperactivity
disorder. J Clin Child Adolesc Psychol. 2014;43(4):527-551.
12. Eldevik S, Hastings RP, Hughes JC, Jahr E, Eikeseth S, Cross S. Meta-
analysis of early intensive behavioral intervention for children with
autism. J Clin Child Adolesc Psychol. 2009;38(3):439-450.
13. Rogers SJ, Vismara LA. Evidence-based comprehensive treatments for
early autism. J Clin Child Adolesc Psychol. 2008;37(1):8-38.
14. Rosa-Alcázar AI, Sánchez-Meca J, Gómez-Conesa A, Marín-Martínez F.
Psychological treatment of obsessive-compulsive disorder: a meta-
analysis. Clin Psychol Rev. 2008;28(8):1310 -1325.
15. Lynch TR, Trost WT, Salsman N, Linehan MM. Dialectical behavior ther-
apy for borderline personality disorder. Annu Rev Clin Psychol. 2007;
3:181-205.
16. Matusiewicz AK, Hopwood CJ, Banducci AN, Lejuez CW. The effective-
ness of cognitive behavioral therapy for personality disorders. Psychiatr
Clin North Am. 2010;33(3):657-685.
17. Keel PK, Haedt A. Evidence-based psychosocial treatments for eating
problems and eating disorders. J Clin Child Adolesc Psychol. 2008;
37(1):39-61.
18. Okajima I, Komada Y, Inoue Y. A meta-analysis on the treatment effec-
tiveness of cognitive behavioral therapy for primary insomnia. Sleep Biol
Rhythms. 2011;9 (1):24-34.
19. American Psychological Association, Society of Clinical Psychol-
ogy. Psychological treatments. http://www.div12.org/psychological-
treatments/treatments. Accessed June 2, 2015.
20. Clark DM, Ehlers A, McManus F, et al. Cognitive therapy versus fluox-
etine in generalized social phobia: a randomized placebo-controlled
trial. J Consult Clin Psychol. 2003;71(6):1058-1067.
21. Heuzenroeder L, Donnelly M, Haby MM, et al. Cost-effectiveness of psy-
chological and pharmacological interventions for generalized anxiety
disorder and panic disorder. Aust N Z J Psychiatry. 2004;38(8):602-612.
22. Miklowitz DJ, Scott J. Psychosocial treatments for bipolar disorder: cost-
effectiveness, mediating mechanisms, and future directions. Bipolar
Disord. 2009;11(suppl 2):110 -122.
23. Turner DT, van der Gaag M, Karyotaki E, Cuijpers P. Psychological inter-
ventions for psychosis: a meta-analysis of comparative outcome studies.
Am J Psychiatry. 2014;171(5):523-538.
24. Shaw B, Segal Z. Efficacy, indications, and mechanisms of action of
cognitive therapy of depression. In: Janowsky DS. Psychotherapy Indi-
cations and Outcomes. Washington, DC: American Psychiatric Press;
1999:173-195.
25. Storchheim LF, O’Mahony JF. Compulsive behaviours and levels of belief
in obsessive-compulsive disorder: a case-series analysis of their inter-
relationships. Clin Psychol Psychother. 20 06;13 (1) : 64-79.
26. Cuijpers P, Dekker J, Hollon SD, Andersson G. Adding psychotherapy to
Table 2. Core Components and Characteristics
of Cognitive Behavior Therapy
One 60- to 90-minute session per week, typically for eight
to 12 weeks
Symptom measures are collected frequently
Treatment is goal-oriented and collaborative; patient is
expected to be an active participant
Treatment is focused on changing current problematic or
maladaptive thoughts or behaviors
Weekly homework assignments

Cognitive Behavior Therapy
812 American Family Physician www.aafp.org/afp Volume 92, Number 9
◆
November 1, 2015
pharmacotherapy in the treatment of depressive disorders in adults: a
meta-analysis. J Clin Psychiatry. 2009;70(9):1219-1229.
27. Haby MM, Tonge B, Littlefield L, Carter R, Vos T. Cost-effectiveness
of cognitive behavioural therapy and selective serotonin reuptake
inhibitors for major depression in children and adolescents. Aust N Z J
Psychiatry. 2004;38(8):579-591.
28. Hollon SD, DeRubeis RJ, Evans MD, et al. Cognitive therapy and phar-
macotherapy for depression. Singly and in combination. Arch Gen
Psychiatry. 1992;49(10):774-781.
29. Roshanaei-Moghaddam B, Pauly MC, Atkins DC, Baldwin SA, Stein MB,
Roy-Byrne P. Relative effects of CBT and pharmacotherapy in depression
versus anxiety: is medication somewhat better for depression, and CBT
somewhat better for anxiety? Depress Anxiety. 2011;28(7):560-567.
30. Beck JS. Cognitive Behavior Therapy: Basics and Beyond. 2nd ed. New
York, NY: Guilford Press; 2011.
31. Serfaty MA, Haworth D, Blanchard M, Buszewicz M, Murad S, King M.
Clinical effectiveness of individual cognitive behavioral therapy for
depressed older people in primary care: a randomized controlled trial.
Arch Gen Psychiatry. 2009;66 (12):1332-1340.
32. Vittengl JR, Clark LA, Dunn TW, Jarrett RB. Reducing relapse and recur-
rence in unipolar depression: a comparative meta-analysis of cognitive-
behavioral therapy’s effects. J Consult Clin Psychol. 2007;75(3):475-488.
33. Otto MW, Pollack MH, Sabatino SA. Maintenance of remission fol-
lowing cognitive behavior therapy for panic disorder: possible delete-
rious effects of concurrent medication treatment. Behav Ther. 1996;
27(3):473-482.
34. Dimidjian S, Hollon SD, Dobson KS, et al. Randomized trial of behav-
ioral activation, cognitive therapy, and antidepressant medication in the
acute treatment of adults with major depression. J Consult Clin Psychol.
2006;74(4):658-670.
35. Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens
SP. Cognitive processing therapy for veterans with military-related post-
traumatic stress disorder. J Consult Clin Psychol. 2006;74 (5):898-907.
36. de Arellano MA, Lyman DR, Jobe-Shields L, et al. Trauma-focused
cognitive-behavioral therapy for children and adolescents: assessing
the evidence. Psychiatr Serv. 2014;65 (5):591-602.
37. Foa EB, McLean CP, Capaldi S, Rosenfield D. Prolonged exposure vs sup-
portive counseling for sexual abuse-related PTSD in adolescent girls: a
randomized clinical trial. JAMA. 2013;310(24):2650-2657.
38. Otto MW, Smits JA, Reese HE. Combined psychotherapy and pharma-
cotherapy for mood and anxiety disorders in adults: review and analysis.
Clin Psychol Sci Pract. 20 05;12(1) :72-86.
39. Pilling S, Mayo-Wilson E, Mavranezouli I, Kew K, Taylor C, Clark DM;
Guideline Development Group. Recognition, assessment and treat-
ment of social anxiety disorder: summary of NICE guidance. BMJ. 2013;
346:f2541.
40. Bernardy NC. The role of benzodiazepines in the treatment of posttrau-
matic stress disorder (PTSD). PTSD Res Q. 2013;23(4):1-9. http://www.
quantumunitsed.com/get-material.php?id=316. Accessed June 1, 2015.
41. World Health Organization. Guidelines for the management of condi-
tions specifically related to stress. http://apps.who.int/iris/bitstream/
10665/85119/1/9789241505406_eng.pdf. Accessed June 1, 2015.
