A Randomized Controlled Trial Examining CBT for College Students
With ADHD
Arthur D. Anastopoulos
1
, Joshua M. Langberg
2
, Laura D. Eddy
1
, Paul J. Silvia
3
, and Jeffrey D. Labban
4
1
Department of Human Development and Family Studies, University of North Carolina Greensboro
2
Department of Psychology, Virginia Commonwealth University
3
Department of Psychology, University of North Carolina Greensboro
4
Department of Health and Human Sciences, University of North Carolina Greensboro
Objective: College students with attention deficit/hyperactivity disorder (ADHD) are at increased risk for
numerous educational and psychosocial difficulties. This study reports findings from a large, multisite
randomized controlled trial examining the efficacy of a treatment for this population, known as
ACCESS—Accessing Campus Connections and Empowering Student Success. Method: ACCESS is a
cognitive– behavioral therapy program delivered via group treatment and individual mentoring across
two semesters. A total of 250 students (18 –30 years of age, 66% female, 6.8% Latino, 66.3% Caucasian)
with rigorously defined ADHD and comorbidity status were recruited from two public universities and
randomly assigned to receive ACCESS immediately or on a 1-year delayed basis. Treatment response
was assessed on three occasions, addressing primary (i.e., ADHD, executive functioning, depression,
anxiety) and secondary (i.e., clinical change mechanisms, service utilization) outcomes. Results: Latent
growth curve modeling (LGCM) revealed significantly greater improvements among immediate AC-
CESS participants in terms of ADHD symptoms, executive functioning, clinical change mechanisms, and
use of disability accommodations, representing medium to large effects (Cohen’s d, .39 –1.21). Across
these same outcomes, clinical significance analyses using reliable change indices (RCI; Jacobson &
Truax, 1992) revealed significantly higher percentages of ACCESS participants showing improvement.
Although treatment-induced improvements in depression and anxiety were not evident from LGCM, RCI
analyses indicated that immediate ACCESS participants were less likely to report a worsening in
depression/anxiety symptoms. Conclusions: Findings from this RCT provide strong evidence in support
of the efficacy and feasibility of ACCESS as a treatment for young adults with ADHD attending college.
What is the public health significance of this article?
College students with attention deficit/hyperactivity disorder (ADHD) face numerous challenges in
their daily lives that make it difficult to achieve personal and career goals. Findings from our recently
completed clinical trial show that ACCESS—Accessing Campus Connections and Empowering
Student Success—is a promising new evidence-based treatment that gives college students with
ADHD the knowledge and skills necessary to be more successful.
Keywords: ADHD, college students, cognitive– behavioral therapy, intervention, clinical trial
Supplemental materials: https://doi.org/10.1037/ccp0000553.supp
Arthur D. Anastopoulos X
https://orcid.org/0000-0001-6096-0650
Laura D. Eddy X
https://orcid.org/0000-0001-5059-8344
Jeffrey D. Labban X https://orcid.org/0000-0002-3138-6925
Additional information about ACCESS, including information about
the treatment manual and study-specific measures, can be found at:
https://accessproject.uncg.edu/. The authors wish to disclose the fol-
lowing potential conflicts of interest. Arthur D. Anastopoulos, Joshua
M. Langberg, and Laura D. Eddy are authors on a forthcoming publi-
cation entitled, CBT for College Students with ADHD—A Clinical
Guide to ACCESS. Arthur D. Anastopoulos is also a co-author of the
ADHD Rating Scale–5, a modified version of which was used in this
study. The research reported here was supported by the Institute of
Education Sciences, U.S. Department of Education, through Grant
R305A150207 awarded to the University of North Carolina Greens-
boro. The opinions expressed are those of the authors and do not
represent views of the Institute or the U.S. Department of Education.
We thank the disability, student health, and counseling service staffs at
both universities for their partnership in referring college students to the
study and for providing presentations about their services to study
participants. We would also like to extend a special thank you to Kevin
R. Murphy for his invaluable contributions to the project as a member
of the expert review panel.
Correspondence concerning this article should be addressed to Arthur D.
Anastopoulos, Department of Human Development and Family Studies,
University of North Carolina Greensboro, ADHD Clinic at UNCG, 1100
West Market Street, 3rd Floor, Greensboro, NC 27402, United States.
Email: [email protected]
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
Journal of Consulting and Clinical Psychology
© 2021 American Psychological Association 2021, Vol. 89, No. 1, 21–33
ISSN: 0022-006X https://doi.org/10.1037/ccp0000553
21
Attention Deficit/Hyperactivity Disorder (ADHD; American
Psychiatric Association, 2013) is characterized by developmen-
tally inappropriate symptoms of inattention and/or hyperactivity-
impulsivity that remain present and impair functioning across the
life span. Although much has been learned about the impact of
ADHD on children and adults (Barkley, 2015), relatively less
research attention has been directed to the way in which ADHD
unfolds among individuals transitioning through the developmen-
tal period known as emerging adulthood, from 18 to 25 years of
age (Arnett, 2007). Most of what is known about this segment of
the ADHD population comes from studies of young adults attend-
ing 4-year colleges, which in recent years have witnessed dramatic
increases in their enrollments of students with ADHD (Eagan et
al., 2014; Weyandt & DuPaul, 2012). For those individuals with
ADHD who achieved a level of success during high school that
made postsecondary admission possible, it would seem reasonable
to expect that they might be able to continue displaying educa-
tional success during college. Contrary to this expectation, once
enrolled in college, students with ADHD display significant aca-
demic deficits, including lower end-of-semester grade point aver-
ages (GPAs) and less effective study strategies, relative to their
non-ADHD peers (DuPaul et al., 2018; Gormley et al., 2019).
Although the directionality of the association is unclear, up to 55%
of the ADHD college student population may also display comor-
bid psychiatric disorders, most often involving active depressive
(32.3%) or anxiety (28.6%) disorders (Anastopoulos et al., 2018).
Additional impairment has been reported in terms of poorer ad-
justment to college (Blasé et al., 2009) and an overall lower quality
of life (Pinho et al., 2019). Together, such findings may help to
explain why college students with ADHD are more likely to be
placed on academic probation, to take longer to complete their
degrees, and to drop out of college (Barkley et al., 2008; DuPaul
et al., 2018; Hechtman, 2017).
Conceptually, it has been suggested that such difficulties are set
in motion by a “perfect storm” of life circumstances that converge
following the transition from high school into college (Anastopou-
los & King, 2015). Upon enrolling in college, all students face
increased demands for self-regulation, not only with respect to
educational matters but also in terms of various personal and social
responsibilities. This developmental transition is normative and
often the reason why many first-year students, whether they have
ADHD or not, experience trouble adjusting to college. For students
with ADHD, navigating this developmental transition is substan-
tially more challenging, in large part due to their lack of age-
appropriate self-regulation abilities (Barkley, 2015; Fleming &
McMahon, 2012). Further complicating matters is the fact that
many external supports that were in place prior to college, such as
parental monitoring and school-based 504 accommodations, are no
longer available (Meaux et al., 2009).
To reduce risk for negative outcomes, it is critically important
for college students with ADHD to have ready access to treatment.
On many college campuses, disability service accommodations are
the primary mechanism by which students with ADHD receive
assistance (Wolf et al., 2009). Unfortunately, many college stu-
dents choose not to use such services (Fleming & McMahon,
2012). Moreover, when used alone, disability accommodations
appear to produce minimal long-term benefits (e.g., Lewandowski
et al., 2013; Miller et al., 2015) and do not directly address
co-occurring executive functioning deficits (Antshel et al., 2014)
and psychiatric disorders (Anastopoulos et al., 2018). Stimulant
medication is another treatment option that has been well estab-
lished in children and adults (Barkley, 2015), but research address-
ing its use with college students has been limited to only one
clinical trial (DuPaul et al., 2012). Despite this study’s promising
results, showing that lisdexamfetamine dimesylate reduced ADHD
symptoms and improved executive functioning, additional medi-
cation trials are needed to evaluate efficacy in conjunction with
safety concerns, including the risk for misuse, abuse, and diversion
on college campuses (Rabiner et al., 2009).
More recently, psychosocial interventions for college students
with ADHD have been developed and pilot tested (He & Antshel,
2017). These investigations incorporate a diverse array of thera-
peutic perspectives, including cognitive– behavioral therapy (CBT;
LaCount et al., 2015; Van der Oord et al., 2020), coaching (Prevatt
& Yelland, 2015), dialectical behavior therapy (Fleming et al.,
2015), mindfulness-based cognitive therapy (Gu et al., 2018),
self-monitoring (Scheithauer & Kelley, 2017), and organization,
time management, and planning skills training (OTMP; LaCount et
al., 2018).
Findings from these initial investigations have consistently re-
vealed significant improvements in primary ADHD symptoms,
most often involving inattention (Fleming et al., 2015; Gu et al.,
2018; LaCount et al., 2015; LaCount et al., 2018,). Less often,
improvements in self-reported executive functioning (Fleming et
al., 2015) and symptoms of depression and anxiety (Gu et al.,
2018) have been observed. Although not routinely assessed, im-
provements in educational functioning have been reported, includ-
ing decreases in self-reported academic impairment (LaCount et
al., 2018), gains in self-reported learning strategies (LaCount et al.,
2015; Prevatt & Yelland, 2015) and increased use of disability
services and other campus resources (Anastopoulos & King,
2015). Notably, corresponding improvements in GPA have not
been reliably demonstrated (Fleming et al., 2015; Gu et al., 2018;
LaCount et al., 2018).
Taken together, results from this emerging literature offer much
promise for the role that psychosocial interventions, especially
CBT programs, may play in the overall clinical management of
college students with ADHD. At the same time, it is necessary to
acknowledge that reported findings have been inconsistent across
investigations, which limits conclusions about efficacy. Given that
programmatic research in this area has been lacking, many of these
inconsistent findings are likely attributable to methodological lim-
itations and differences across studies (He & Antshel, 2017).
These limitations include, for example, the use of small samples
(n ⬍ 60) drawn from single-site university settings. Diagnostic
rigor has typically been lacking, with many studies relying upon
either symptom counts from a single rating scale or self-report of
prior ADHD diagnoses as the basis for determining participants’
ADHD status. Although co-occurring psychiatric conditions are
common among individuals with ADHD, their presence has either
not been addressed or addressed on a very limited basis. Additional
cross-study differences are evident with respect to the format (i.e.,
group vs. individual) and number (i.e., 3–10) of treatment sessions
offered, as well as the duration of treatment (i.e., 1–3 months).
Furthermore, measures assessing clinical change mechanisms are
rarely included; thus, the conceptual underpinnings of these inter-
ventions are not well understood. Also limited is our understanding
of the persistence of therapeutic improvements beyond active
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
22
ANASTOPOULOS, LANGBERG, EDDY, SILVIA, AND LABBAN
treatment, with only a few studies reporting follow-up assessments
of relatively short duration (i.e., 3 months).
The present study reports findings from a large-scale, multisite
randomized controlled trial (RCT) examining the efficacy of the
CBT program known as ACCESS—Accessing Campus Connec-
tions and Empowering Student Success (Anastopoulos & King,
2015; Anastopoulos et al., 2020). ACCESS incorporates elements
of empirically supported adult CBT programs (Safren et al., 2005;
Solanto, 2011), adapted to the developmental needs of emerging
adults with ADHD in college. ACCESS was originally developed,
refined, and pilot tested in an open clinical trial involving 88
college students with rigorously defined ADHD (Anastopoulos &
King, 2015). An iterative process was used to determine optimal
mode of delivery (e.g., number and length of treatment sessions).
In its current and final form, ACCESS is delivered across two
consecutive semesters, the first of which is an intensive 8-week
active phase, followed by a less intensive semester-long mainte-
nance phase in which treatment is gradually faded. In each phase,
treatment is delivered in both a group and individual mentoring
format. The active phase includes eight weekly group sessions,
each of which is 90 min in length. Concurrent with these group
sessions are weekly individual mentoring sessions, each of which
is approximately 30 min in length. The purpose of individual
mentoring is threefold: to reinforce what the student learns in the
CBT group; to assist the student in establishing personal goals and
monitoring progress; and to help the student make connections
with campus resources as needed (e.g., accommodations, counsel-
ing, medication). As part of the process of fading treatment during
the maintenance phase, one 90-min booster group session is of-
fered at the start of the semester, along with up to six 30-min
individual mentoring sessions that can be scheduled flexibly
throughout the semester at times best meeting participant needs.
Both treatment delivery formats are used to address the goal of
the ACCESS program—namely, to give college students with
ADHD the knowledge and skills necessary to be successful in their
daily life functioning. Specifically, ACCESS is designed to: (a)
give college students a developmentally appropriate understanding
of their own ADHD via a more intensive “dosage” of ADHD
knowledge than is delivered in adult CBT programs (Safren et al.,
2005; Solanto, 2011); (b) improve organization, time management,
and other behavioral strategies that target executive functioning
deficits commonly found among individuals with ADHD; and (c)
increase adaptive thinking skills via cognitive therapy strategies to
address co-occurring depression and anxiety features that are fre-
quently comorbid with ADHD (Anastopoulos et al., 2018). In
contrast with the sequential way in which adult CBT programs
(Safren et al., 2005) deliver these treatment modules (i.e., ADHD
knowledge ¡ behavioral strategies ¡ cognitive therapy),
ACCESS delivers them simultaneously in an integrated fashion,
focused on a common theme (e.g., academic functioning), in each
of the eight active phase group sessions (see Figure 1). The
underlying premise of ACCESS is that improvement in ADHD
knowledge, behavioral strategies, and adaptive thinking skills—
that is, the hypothesized clinical change mechanisms—will facil-
itate improvements in multiple domains of daily life functioning
negatively impacted by ADHD.
Results from our completed open clinical trial revealed statisti-
cally significant improvements in ADHD symptoms, executive
functioning, levels of depression and anxiety, and the number of
semester credit hours attempted and earned (Anastopoulos et al.,
2020). Of note, such improvements were evident at the end of the
active phase and maintained throughout the maintenance phase, 5
to 7 months after treatment started.
The current study builds upon these promising findings and
addresses many of the previously mentioned limitations in the
literature. For example, the current RCT used a large sample of
250 college students with rigorously defined ADHD and comorbid
psychiatric diagnoses drawn from two university settings. Partic-
ipants were randomly assigned either to a group receiving the
ACCESS treatment immediately or to a Delayed Treatment Con-
trol (DTC) condition receiving treatment 1 year later. In contrast
with other CBT programs, ACCESS incorporates concurrent de-
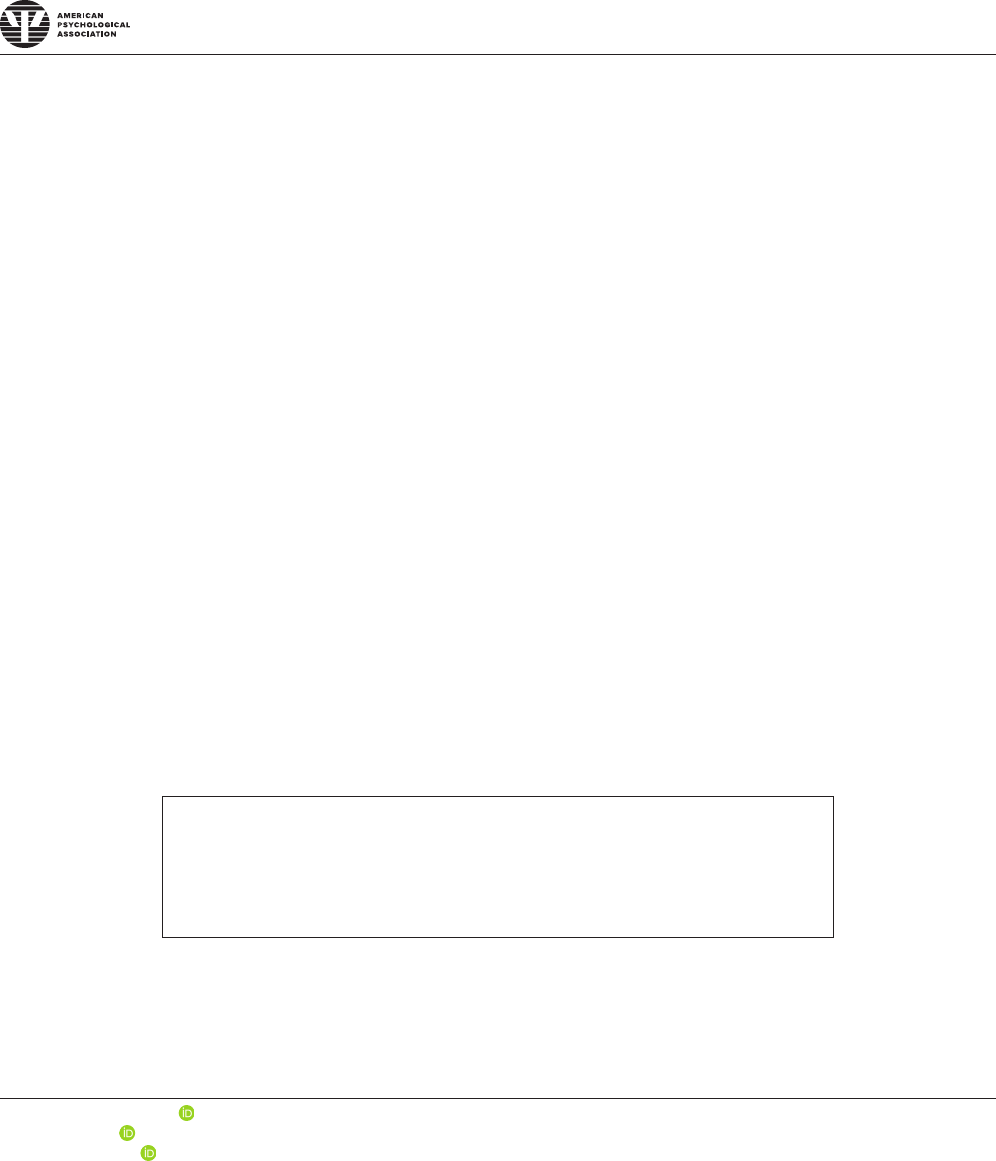
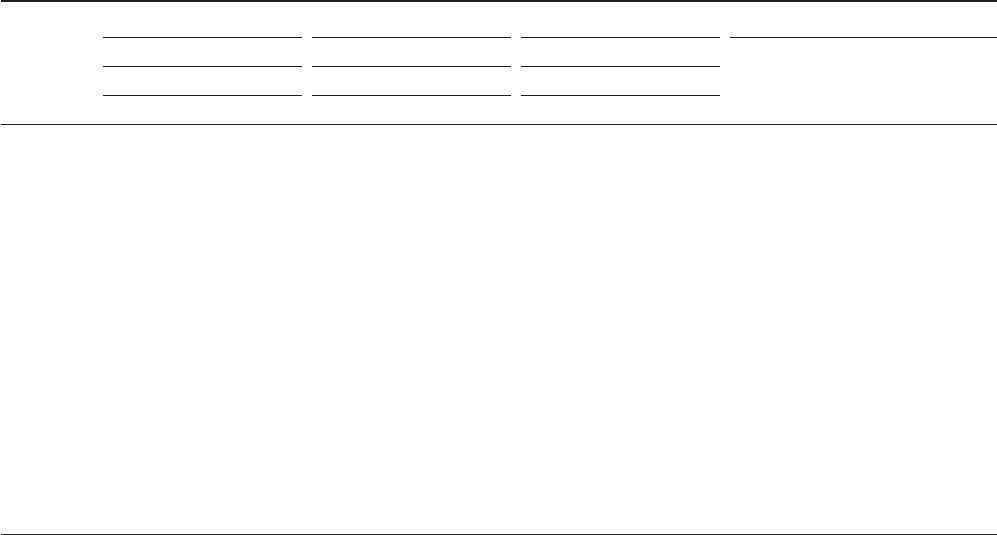
Figure 1
Weekly CBT Group Session Content During the Active Phase of the ACCESS Intervention
Week 1 Week 2 Week 3 Week 4 Week 5 Week 6 Week 7 Week 8
ADHD
Knowledge
Primary
Symptoms
Causes Assessment
School &
Daily
Functioning
Emotions
&Risk-
Taking
Medication
Management
Psychosocial
Treatment
Long-Term
Outlook
Behavioral
Strategies
Campus
Resources
Planners &
To-Do Lists
Getting
Organized
Attending
Classes
Effective
Studying
Long-Term
Projects
Social
Relationships
Long-Term
Goals
Adaptive
Thinking
Basic
Principles
Maladaptive
Thinking
Adaptive
Thinking
Managing
Schoolwork
Handling
Emotions
Adhering to
Treatment
Social
Relationships
Relapse
Prevention
Note. CBT ⫽ cognitive– behavioral therapy; ADHD ⫽ attention deficit/hyperactivity disorder.
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
23
CBT FOR COLLEGE STUDENTS WITH ADHD
livery of group and individual sessions, which affords participants
exposure not only to the unique benefits of each treatment modal-
ity, but also to a greater total number of therapeutic contacts (i.e.,
21–25), thereby increasing the intensity of treatment. To better
address the chronic nature of ADHD, participants remain in con-
tact with ACCESS staff for a substantially longer duration (i.e.,
6 –7 months across two semesters) than is offered in similar
interventions. To assess the stability of therapeutic change, out-
come was assessed on three occasions, spanning a full academic
year. Also included were measures of hypothesized clinical change
mechanisms that have direct bearing on the construct validity of
the design.
The purpose of this article is to present RCT findings that
directly address the efficacy of ACCESS across its entire two-
semester long delivery. Given the large number of outcome vari-
ables included in the RCT, the focus of this initial efficacy article
is limited to treatment-induced changes in: (a) primary outcomes
addressing ADHD symptoms, executive functioning (EF), and
co-occurring symptoms of depression and anxiety, and (b) second-
ary outcomes related to hypothesized clinical change mechanisms
and treatment service utilization. It was hypothesized that, relative
to the DTC condition, participants receiving ACCESS would dis-
play significantly greater improvements in their ADHD symptoms,
EF, co-occurring depression and anxiety symptoms, hypothesized
clinical change mechanisms, and treatment service utilization after
both phases (i.e., active and maintenance) of treatment were com-
pleted. Using reliable change indices (Jacobson & Truax, 1992)to
address the clinical significance of these findings, it was also
expected that higher percentages of ACCESS participants would
show reliable postintervention improvements in these same out-
come domains relative to DTC participants.
Method
Participants
Participants for this study were recruited from two large, public
universities in the southeastern United States that serve large
numbers of first-generation college students and students of color.
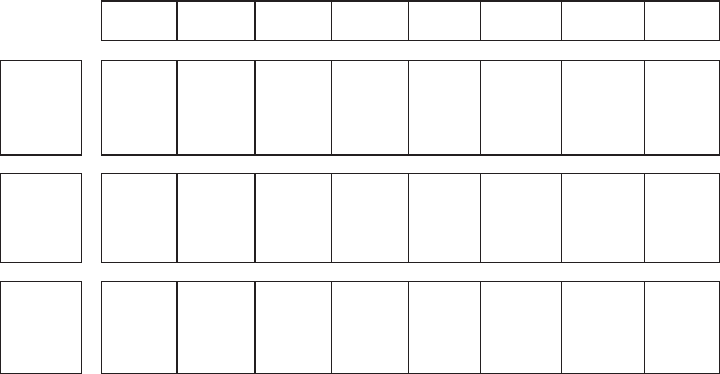
As shown in Figure 2, a total of 361 students were initially
consented into the project and screened for eligibility. Eighty-one
were deemed ineligible, either because they did not meet research
criteria for ADHD or because they displayed a co-occurring psy-
chiatric condition (e.g., autism spectrum disorder, bipolar disorder,
obsessive– compulsive disorder) requiring treatment that went be-
yond the scope of the intervention. The remaining 280 participants
meeting eligibility criteria were randomly assigned to receive
ACCESS immediately or on a 1-year delayed basis in the DTC
group. Random assignment was stratified by medication status to
ensure that equivalent numbers of participants taking ADHD med-
ication were assigned to each group condition. Thirty eligible
students assigned to the immediate ACCESS group could not
begin treatment due to class and job schedules that conflicted with
planned group meeting times. This resulted in a final sample of
250 participants, including 165 females (66%) and 85 males
(34%), ranging in age from 18 to 30 years (M ⫽ 19.7, 8.4% ⱖ 23)
and representing a cross-section of postsecondary education levels
(i.e., 47.6% first-year students, 16.4% sophomores, 26.4% juniors,
9.6% seniors). A significant number of these students had experi-
enced academic difficulties prior to enrolling in college, with
26.8% having received at least one D or F grade in high school.
Another 38.4% reported having to work part-time to support
themselves financially while attending college. Approximately
6.8% of the participants reported having Hispanic/Latino back-
grounds; 66.3% identified as Caucasian, 14.2% as African Amer-
ican, 5.3% as Asian, 10.6% as multiracial, and 3.3% as other or not
reported.
A multigating, multimethod, multi-informant assessment ap-
proach (Ramsay, 2015) was used to determine ADHD and comor-
bidity status. Potential participants were initially screened based on
their responses to the ADHD Rating Scale-5 (DuPaul et al., 2016).
Students endorsing four or more symptoms of either inattention
and/or hyperactivity-impulsivity were scheduled for further eval-
uation, which included: a semistructured interview assessing cur-
rent ADHD symptoms and their associated impairment; self-report
rating scales assessing current and childhood symptoms of ADHD;
a structured interview addressing other psychiatric disorders that
may be exclusionary or co-occurring with ADHD; and self-report
ratings of depression and anxiety symptoms. Family, school, and
social background information was also collected, along with prior
mental health evaluation and treatment histories. To increase the
accuracy of addressing the childhood onset criteria, efforts were
made (with consent) to obtain parental ratings of participants’
ADHD symptoms occurring prior to 12 years of age. For a variety
of reasons (e.g., consent withheld, parents not available), it was not
possible to obtain parental ratings for 12.4% of the sample, but this
did not preclude participation in the study. All collected evaluation
data were forwarded to a panel of three ADHD experts (i.e., the
two study principal investigators and a nationally recognized adult
ADHD clinical consultant), who independently reviewed each case
to determine if criteria for ADHD and/or other psychiatric disor-
ders had been met, as defined in the Diagnostic and Statistical
Manual of Mental Disorders–Fifth Edition (DSM–5; American
Psychiatric Association, 2013). Final determination of ADHD and
psychiatric comorbidity status required unanimous panel agree-
ment.
Included among the 250 participants in the final sample were
58.4% who received an ADHD Combined presentation diagnosis
and 41.6% who displayed an ADHD Predominantly Inattentive
presentation. Although it was not a requirement for inclusion in the
study, 66.4% of these participants reported having been previously
diagnosed with ADHD; another 24.4% reported histories of being
strongly suspected of having ADHD—that is, significant others
(e.g., parents, teachers, friends) repeatedly raising the possibility
that the participant might have ADHD. Sixty percent also met
DSM–5 criteria for at least one psychiatric diagnosis co-occurring
with ADHD, most often involving a current anxiety or depressive
disorder. For clinical and ethical reasons, students in both condi-
tions could participate in the study regardless of whether they were
receiving other forms of treatment. At the time they were randomly
assigned to a group, nearly half (47.2%) of the participants in the
final sample were taking medication for ADHD; 27.7% were
taking medication for other medical and mental health conditions,
including 10.8% for the treatment of depression and anxiety.
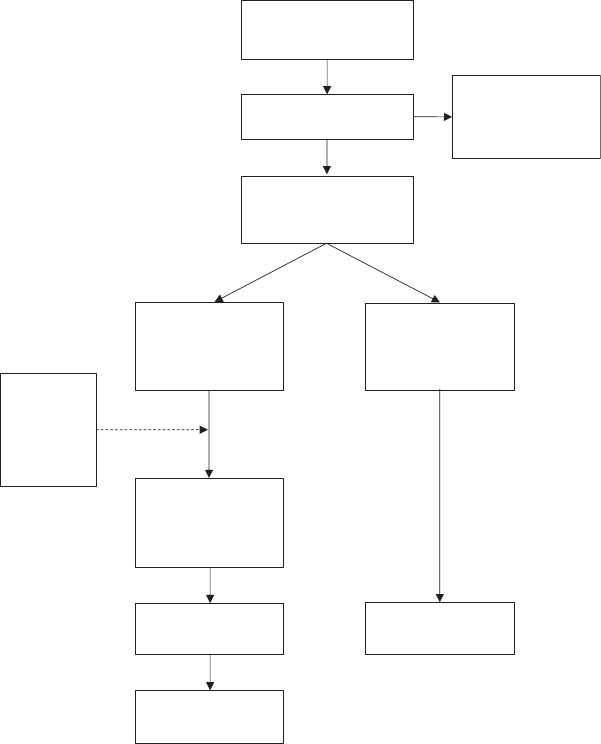
As shown in Table 1, the two groups (immediate ⫽ 119, DTC ⫽
131) were statistically equivalent at pretreatment across these
demographic and clinical variables of interest.
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
24
ANASTOPOULOS, LANGBERG, EDDY, SILVIA, AND LABBAN
Diagnostic Measures
Semi-Structured Interview for Adult ADHD
The Semi-Structured Interview for Adult ADHD was devel-
oped specifically for this study because it allowed for a more
thorough and simultaneous assessment of symptoms and
ADHD-specific impairment. For each of the 18 ADHD symp-
toms, respondents rated not only the frequency of occurrence
but also the degree to which there was associated impairment in
daily functioning. In contrast with the fixed way in which
ADHD symptoms are listed in rating scales, interviewers were
allowed to give developmentally appropriate parenthetical de-
scriptions of ADHD symptoms to increase participant under-
standing of the questions being asked. Additional questioning is
directed to the other DSM–5 criteria addressing duration, age of
onset, and exclusionary conditions. Preliminary (unpublished)
analyses indicate that this interview possesses satisfactory re-
liability (coefficient ␣ from .84 to .90) and is highly correlated
with CAARS-S:L symptom dimensions (from .78 to .84). In-
formation from this interview was used in combination with
other assessment data to determine ADHD status.
ADHD Rating Scale-5
The ADHD Rating Scale-5 (ARS-5; DuPaul et al., 2016)isan
18-item questionnaire that possesses excellent reliability (coeffi-
cient ␣ from .89 to .94) and validity and has been used widely in
research and practice. The self-report and parent-report versions of
the ARS-5, which address current functioning, were modified to
include a second column for rating each symptom during child-
hood. Together, these self-report and parent ratings were used to
provide a more specific estimation of the onset and persistence of
ADHD across the life span.
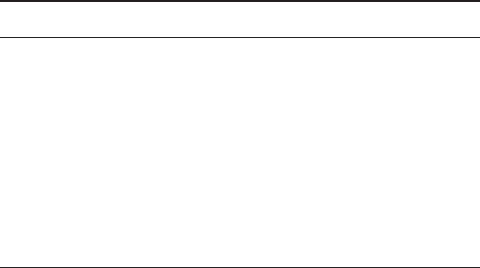
Figure 2
Consort Diagram Showing Flow of Participants Through Clinical Trial. Drop-
Out Rates Were Comparable for the Immediate (20.2%) and Delayed Treatment
Groups (22.1%) at Posttreatment (Postmaintenance Phase). Drop-Outs Did Not
Differ From Completers on Any Pretreatment Demographic, Primary Outcome,
or Secondary Outcome
Assessed for eligibility
(N = 361)
Excluded; did not
meet eligibility
criteria
(n= 81)
Randomized
(n = 280)
Post-treatment
(n = 95)
Assigned to
immediate
intervention
(n= 149)
Assigned to
delayed
intervention
(n= 131)
Post-treatment
(n = 102)
Follow-up
(n = 92)
Enrollment
Attended at least
one treatment
session
(n = 119)
Unable to
participate;
scheduling
conflicts
(n = 30)
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
25
CBT FOR COLLEGE STUDENTS WITH ADHD
Structured Clinical Interview for DSM–5: Research
Version (SCID-5-RV)
The SCID-5-RV (First, Williams, Karg, & Spitzer, 2015)
screeners for the mood, anxiety, trauma, and substance use mod-
ules (coefficient ␣ from .85 to .98) were initially administered to
all participants, after which complete modules were given as
needed for disorders suspected of being present. Information gath-
ered from the SCID-5-RV was used to identify psychiatric condi-
tions that could either rule out an ADHD diagnosis or co-occur
with ADHD, as determined by the expert panel.
Primary Outcome Measures
Conners Adult ADHD Rating Scale, Self-Report, Long
Version (CAARS-S:L)
The CAARS-S:L (Conners et al., 2006) is a widely used, psy-
chometrically sound (coefficient ␣ from .73 to .84) measure of
ADHD in adults. The DSM–IV Inattentive (IN), Hyperactive-
Impulsive (HI), and Total scores were used to assess treatment-
related changes in ADHD symptoms.
Behavior Rating Inventory of Executive Function–Adult
Version (BRIEF-A)
The BRIEF-A (Roth et al., 2005) is a 75-item psychometrically
sound (coefficient ␣⫽.96) self-report measure that generates nine
clinical scales (e.g., Self-Monitoring, Planning, Working Memory,
Emotional Control), as well as three composite scales—the Be-
havior Regulation Index (BRI), Metacognition Index (MCI), and
overall Global Executive Composite (GEC)—which were used to
assess executive functioning (EF) deficits. Higher scores on these
BRIEF-A composite scales indicate poorer EF.
Beck Depression Inventory, Second Edition (BDI-II)
The BDI-II (Beck et al., 1996) is a psychometrically sound
(coefficient ␣⫽.93) measure of adult depression that is widely
used in research and clinical practice. The BDI-II total score
served as a measure of treatment-induced changes in depressed
mood.
Beck Anxiety Inventory (BAI)
The BAI (Beck & Steer, 1993) is a psychometrically sound
(coefficient ␣⫽.92) measure of anxiety symptoms in adults, used
widely in research and clinical practice. The BAI total score was
used to assess changes in overall levels of anxiety.
Secondary Outcome Measures
Because we were not aware of existing measures for evaluating
hypothesized clinical change mechanisms and participant service
utilization, we assessed these constructs using procedures that we
developed for this and related studies involving college students
with ADHD.
Test of ADHD Knowledge (TOAK)
The TOAK is a 40-item questionnaire that measures general
knowledge of ADHD. For each item, participants respond to
statements about ADHD (e.g., “Hereditary factors play a major
role in determining if someone will develop ADHD”) with
“agree,” “disagree,” or “not sure.” Correctly endorsed “agree” and
“disagree” items are summed to yield a total score, with higher
scores indicating greater knowledge of ADHD. Preliminary (un-
published) findings based on the current sample indicate that the
TOAK possesses excellent internal consistency (coefficient ␣⫽
.86) and demonstrates evidence of convergent validity.
Strategies for Success (SFS)
The SFS contains 18 items that assess self-reported use of
behavioral strategies (e.g., “Doing the most important tasks first”)
for managing academic work in college. Respondents indicate how
adeptly they use these strategies on a 5-point scale, with 1 indi-
cating not well and 5 indicating very well. Items are summed to
yield a total score, with higher scores indicating more frequent
behavioral strategy use. Initial (unpublished) findings from the
current sample suggest that the SFS possesses excellent internal
consistency (coefficient ␣⫽.84).
ADHD Cognitions Scale–College Version (ACS-CV)
The ACS-CV is a 12-item questionnaire that assesses self-
reported frequency of ADHD-related cognitions (e.g., “My work is
better if I wait until the last minute”). Each item is rated on a
5-point scale, and ratings for all 12 items are summed to create a
total ACS-CV score, with higher scores reflecting more frequent
engagement in maladaptive thinking patterns. The ACS-CV uses
many of the same items found in the 7-item ACS developed for
older adult populations (Knouse et al., 2019). For college students,
a psychometrically sound 12-item version was found to be more
Table 1
Pretreatment Demographic and Clinical Characteristics
by Group
Variable
ACCESS DTC
M (SD) M (SD)
Age (years) 19.7 (2.2) 19.6 (2.1)
CAARS Total ADHD score 34.4 (9.2) 34.7 (8.9)
%%
Sex (female) 64.7 67.2
Race: Caucasian 66.1 66.4
African-American 11.9 16.4
Asian 5.1 5.5
More than one race 11.9 9.4
Other/not reported 5.1 2.4
Ethnicity: Hispanic 7.0 6.6
First year students 49.6 45.8
Comorbidity status 62.2 58.0
ADHD: Combined 58.8 58.0
Predominantly inattentive 41.2 42.0
ADHD medications 53.3 41.7
Other medications 26.1 29.1
Note. ACCESS ⫽ immediate treatment; DTC ⫽ Delayed Treatment
Control; ADHD ⫽ attention deficit/hyperactivity disorder; CAARS ⫽
Conners Adult ADHD Rating Scale; Comorbidity status ⫽ presence of any
non-ADHD psychiatric disorder; ADHD medication status ⫽ reported use
of medication to treat ADHD; Other medication status ⫽ reported use of a
medication to treat other medical/mental health conditions.
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
26
ANASTOPOULOS, LANGBERG, EDDY, SILVIA, AND LABBAN
appropriate, with satisfactory internal consistency (coefficient ␣⫽
.77) and evidence of convergent and divergent validity.
Services for College Students Questionnaire (SCSQ)
The SCSQ is a self-report descriptive measure that monitors
participant use of campus support services (e.g., disability accom-
modations) and other treatments (e.g., ADHD medication). For
each service, participants first indicate whether they receive this
service and then provide information about its frequency, duration,
and effectiveness. In this study, participant use of disability ac-
commodations, ADHD medication, medication for other medical/
mental health conditions, and counseling was assessed.
Procedure
Students were recruited from multiple sources, including vari-
ous campus support units (e.g., disability services, student health
services, first-year summer orientation sessions, and campus fli-
ers). All potential participants were made aware that this was a
clinical trial for individuals with ADHD, and that ADHD status
would be evaluated and confirmed prior to entry into the trial.
Interested students contacted the project coordinators at each site
and were initially screened for study eligibility by phone. Poten-
tially eligible participants subsequently underwent a more com-
prehensive evaluation, during which information pertinent to de-
termining eligibility for the study, as well as pretreatment outcome
data, were collected.
Recruitment was ongoing, and ACCESS was delivered to five
successive cohorts of participants across consecutive semesters
from the fall of 2015 through the spring of 2018. Fall cohorts ran
from early September through mid-November; spring cohorts from
early February into mid-April. Treatment outcome data were col-
lected from both groups on three occasions: within 2 weeks prior
to beginning active treatment, immediately after active treatment,
and in the final 2–3 weeks of the maintenance phase semester.
While waiting to participate in ACCESS on a 1-year delayed basis,
DTC participants were permitted to receive treatment as usual.
CBT group and mentoring sessions were conducted in campus-
based clinic settings. Every effort was made to run CBT group
meetings at times that maximized attendance; some students (n ⫽
30) could not participate due to scheduling conflicts (e.g., classes,
jobs). On average, four to six students participated in the CBT
group portion of ACCESS. Groups were conducted using a
discussion-based format to encourage active participation, and
participants received written handouts summarizing important ses-
sion content. Guest speakers from various campus support units
(e.g., disability services, student health) met briefly with the
groups to describe and answer questions about their services.
Mentoring sessions were generally conducted in person within a
few days following the corresponding group session; occasionally,
when in-person sessions were not feasible (e.g., illness), mentoring
was instead conducted by phone.
Graduate student research assistants and one master’s-level li-
censed professional counselor served as group leaders and men-
tors. Prior to being in the study, all received extensive training that
included assigned readings, group discussions, observations, and
role playing. Supervision was provided to group leaders and men-
tors throughout the study by licensed doctoral-level clinical psy-
chologists. Treatment fidelity was further enhanced through use of
a treatment manual containing detailed session-by-session outlines
that guided group leaders and mentors in their delivery of
ACCESS. All treatment sessions were audio recorded, and 20% of
these were randomly selected and reviewed for treatment fidelity
by the group and mentor supervisors. Overall adherence to the
content of treatment sessions was excellent, with fidelity ratings of
96.4 and 95.6% obtained for the group and mentoring sessions,
respectively.
All study procedures were approved annually by each universi-
ty’s Institutional Review Board. In addition to receiving monetary
compensation for completing measures, participants were given a
written summary of their screening evaluation results, which could
be used as documentation for receiving campus support and treat-
ment (e.g., accommodations, medication).
Results
Data Analytic Plan
Latent growth curve models, which allow for analysis of cases
with missing data, were estimated to evaluate how treatment
condition (immediate vs. delayed) influenced change over time.
The models were estimated in Mplus 8.1 using maximum likeli-
hood estimation with robust standard errors, which incorporates a
model-based method for estimating parameters despite missing
data (Enders, 2010). Scores for the three time points (preactive,
postactive, and postmaintenance) served as the indicators. Latent
intercept and slope factors were specified and allowed to covary.
For the intercept, the three factor loadings were set to 1. For the
slope, the first indicator (preactive) was fixed to zero, the second
indicator was freely estimated, and the final indicator (postmain-
tenance) was fixed to 1. In this specification, the intercept value
reflects initial preactive status, and the slope value reflects total
growth from preactive (Time 1, coded 0) to postmaintenance
(Time 3, coded 1).
A multiple-group framework was used to evaluate differential
change over time. The immediate ACCESS and DTC conditions
were specified as the two groups, and Wald tests of model con-
straints were used to test whether the slope means differed signif-
icantly between the two groups. Rarely were there significant
effects of treatment condition on intercept values (i.e., pretreat-
ment scores), consistent with random assignment to condition, and
so these effects were omitted from the main text for clarity.
Because the slopes were constrained to be equal, a significant
model test indicates a rejection of the null hypothesis of equal
slopes in the two group conditions. Within each group, the residual
variances of the intercept and slope, as well as their residual
covariance, were freely estimated. The residual variances of the
slopes tended to be small, and in a handful of cases (e.g., BDI-II)
they were fixed to 0 to facilitate convergence to proper solutions.
The residual variances of the three indicators were constrained to
be equal within each group to reflect homoscedasticity (Preacher et
al., 2008). Initial growth analyses indicated that site differences
had no impact on the trajectories for either group; thus, site was not
included in the final growth models. Model fit for the multiple
group models is displayed in Table 2, with the data reported in the
original, unstandardized metric. Reported below for each outcome
are effect sizes, expressed in the Cohen’s d metric, representing the
magnitude of the difference in slopes between the ACCESS and
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
27
CBT FOR COLLEGE STUDENTS WITH ADHD
DTC conditions (i.e., the effect of condition on change). For the
purposes of interpretation, Cohen’s d values on the order of .20,
.50, and .80 were considered small, medium, and large effects,
respectively.
Primary Outcomes
ADHD Symptoms
The immediate ACCESS (b ⫽⫺6.16, SE ⫽ .82, p ⬍ .001) and
DTC (b ⫽⫺2.90, SE ⫽ .66, p ⬍ .001) groups showed significant
declines in overall ADHD symptomatology as measured by
CAARS Total ADHD scores, with the decline being significantly
greater in the ACCESS condition, Wald (1) ⫽ 9.78, p ⫽ .002, d ⫽
.39 [.15, .65]. The ACCESS (b ⫽⫺4.83, SE ⫽ .52, p ⬍ .001) and
DTC (b ⫽⫺3.32, SE ⫽ .38, p ⬍ .001) groups also showed
significant declines in inattention symptoms as measured by
CAARS IN scores, with a significantly larger decline observed
among ACCESS participants, Wald (1) ⫽ 16.08 p ⬍ .001, d ⫽ .50
[.25, .76]. As shown in Figure S1 (in the online supplemental
materials), these reductions in ADHD symptoms were evident at
the end of the active phase and remained stable throughout the
maintenance phase of the intervention. In contrast with the mar-
ginal decline in hyperactive-impulsive symptoms (CAARS HI
scores) shown by the DTC condition (b ⫽⫺.64, SE ⫽ .34, p ⫽
.060), the ACCESS group showed a significant decline
(b ⫽⫺1.32, SE ⫽ .43, p ⫽ .002); the slopes, however, did not
differ between these groups, Wald (1) ⫽ 1.50, p ⫽ .220, d ⫽ .16
[⫺.09, .41].
Executive Functioning
In terms of overall EF deficits as measured by BRIEF-A GEC
scores, the DTC condition showed a marginal decline
(b ⫽⫺3.31, SE ⫽ 2.02, p ⫽ .101), whereas the immediate
ACCESS group (b ⫽⫺16.69, SE ⫽ 2.28, p ⬍ .001) showed a
significant decline and its slope was significantly greater than
that of the DTC condition, Wald (1) ⫽ 22.32, p ⬍ .001, d ⫽ .56
[.31, .81]. In contrast with the DTC group that displayed no
change in behavioral regulation deficits as measured by
BRIEF-A BRI scores (b ⫽ .14, SE ⫽ .85, p ⫽ .867), the
ACCESS group (b ⫽⫺4.17, SE ⫽ .98, p ⬍ .001) showed a
significant decline and the slopes differed significantly between
the conditions, Wald (1) ⫽ 10.78, p ⫽ .001, d ⫽ .43 [.17, .68].
Regarding metacognition deficits (BRIEF-A MCI scores), there
were significant declines in both the ACCESS group
(b ⫽⫺11.26, SE ⫽ 1.82, p ⬍ .001) and the DTC condition
(b ⫽⫺3.14, SE ⫽ 1.59, p ⫽ .049), but the decline for ACCESS
participants was significantly greater, Wald (1) ⫽ 18.25, p ⬍
.001, d ⫽ .43 [.18, .68]. For all three BRIEF-A measures, these
improvements in EF were evident at the end of the active phase
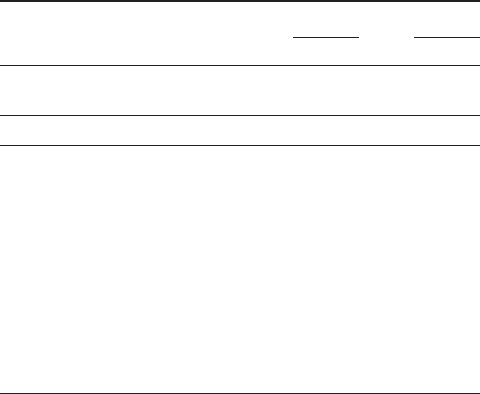
Table 2
Outcome Data and Model Fit Indices
Time 1 Time 2 Time 3 Model fit for multiple group models
Outcome
M (SD) M (SD) M (SD)
2
(df) CFI SRMR
RMSEA
[90% CI]
nnn
ACCESS DTC ACCESS DTC ACCESS DTC
CAARS Total 34.48 (9.16) 34.73 (8.82) 29.64 (9.28) 31.54 (10.43) 28.46 (9.48) 31.68 (9.48) 9.31 (7) .99 .12 .05 [.00, .13]
117 130 111 109 95 102
IN 19.93 (4.57) 20.36 (4.45) 16.25 (5.20) 18.22 (5.70) 15.05 (5.24) 17.86 (5.28) 16.22 (7) .94 .20 .10 [.04, .17]
117 130 111 109 95 102
HI 14.55 (5.74) 14.37 (5.61) 13.39 (5.32) 13.32 (6.23) 13.41 (5.57) 13.81 (5.89) 3.87 (5) 1 .06 .00 [.00, .11]
117 130 111 109 95 102
BRIEF GEC 157.17 (18.13) 155.62 (22.30) 145.86 (25.05) 154.00 (24.46) 140.39 (24.85) 150.01 (24.69) 9.09 (7) .98 .25 .05 [.00, .13]
118 131 113 111 93 100
BRI 60.70 (11.22) 59.40 (11.05) 58.02 (12.28) 59.85 (11.95) 56.88 (11.86) 59.06 (11.95) 3.38 (7) 1 .10 .00 [.00, .06]
118 131 113 111 93 100
MCI 95.62 (14.71) 95.87 (14.84) 87.58 (15.23) 94.15 (15.18) 83.51 (15.07) 90.93 (15.48) 7.05 (5) .96 .07 .06 [.00, .15]
118 131 113 111 93 100
BDI-II 14.60 (10.55) 14.82 (10.57) 12.97 (9.98) 18.47 (11.97) 13.12 (11.39) 16.19 (11.62) 7.80 (7) .99 .08 .03 [.00, .12]
119 131 113 113 95 103
BAI 13.67 (11.79) 12.15 (10.29) 14.32 (11.40) 14.65 (11.38) 12.27 (10.53) 14.29 (12.04) 8.28 (5) .98 .03 .07 [.00, .16]
119 131 113 113 94 102
TOAK 20.86 (6.19) 20.85 (6.23) 29.93 (4.86) 22.70 (5.68) 29.03 (5.00) 23.15 (5.63) 17.91 (5) .93 .08 .14 [.08, .22]
119 129 113 110 94 103
SFS 46.74 (10.97) 44.74 (11.00) 61.16 (11.64) 48.84 (12.09) 61.18 (12.27) 49.58 (13.58) 6.33 (5) .99 .09 .05 [.00, .14]
119 131 112 113 93 104
ACS-CV 36.27 (7.88) 36.03 (8.23) 32.93 (7.84) 35.77 (7.91) 31.91 (8.13) 35.54 (8.71) 4.43 (5) 1 .07 .00 [.00, .12]
119 131 110 113 95 103
Note. Outcome data reported in the original, unstandardized metric; CFI ⫽ comparative fit index; SRMR ⫽ standardized root mean square residual;
RMSEA ⫽ root mean square error of approximation; ACCESS ⫽ immediate treatment; DTC ⫽ Delayed Treatment Control; CAARS total ⫽ Conners Adult
ADHD Rating Scale total score; IN ⫽ CAARS inattention; HI ⫽ CAARS hyperactivity-impulsivity; BRIEF GEC ⫽ Behavioral Rating Inventory of
Executive Functioning Global Executive Composite; BRI ⫽ BRIEF Behavior Regulation Index; MCI ⫽ BRIEF Metacognition Index; BDI-II ⫽ Beck
Depression Inventory–II; BAI ⫽ Beck Anxiety Inventory; TOAK ⫽ Test of ADHD Knowledge; SFS ⫽ Strategies for Success; ACS-CV ⫽ ADHD
Cognitions Scale–College Version.
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
28
ANASTOPOULOS, LANGBERG, EDDY, SILVIA, AND LABBAN
and remained stable throughout the maintenance phase of AC-
CESS (see Figure S2 in the online supplemental materials).
Emotional Functioning
Analyses of the BDI-II revealed no significant reductions in
depression symptoms for either the ACCESS (b ⫽⫺.77, SE ⫽
.74, p ⫽ .297) or DTC groups (b ⫽ 1.81, SE ⫽ 1.14, p ⫽ .111),
and the slopes did not differ significantly, Wald (1) ⫽ 2.13, p ⫽
.145, d ⫽ .24 [⫺.01, .49]. Analyses of BAI scores indicated that
there was a significant increase in anxiety for the DTC group (b ⫽
2.78, SE ⫽ .98, p ⫽ .005), but no change in the ACCESS condition
(b ⫽⫺1.10, SE ⫽ 1.16, p ⫽ .346); the slopes between groups
differed significantly, Wald (1) ⫽ 6.22, p ⫽ .013, d ⫽ .33 [.08,
.58]. Although emotional functioning did not improve, it is of
clinical interest to note that depression and anxiety levels seemed
to stabilize for ACCESS participants, while worsening for DTC
participants (see Figure S3 in the online supplemental materials).
Secondary Outcomes
Clinical Change Mechanisms
The immediate ACCESS (b ⫽ 8.29, SE ⫽ .53, p ⬍ .001) and
DTC (b ⫽ 1.99, SE ⫽ .41, p ⬍ .001) groups showed significant
growth in their knowledge of ADHD as measured by TOAK
scores. This increase in ADHD knowledge was significantly
greater among ACCESS participants, Wald (1) ⫽ 102.24, p ⬍
.001, d ⫽ 1.21 [.94, 1.48]. The immediate ACCESS (b ⫽ 14.50,
SE ⫽ 1.33, p ⬍ .001) and DTC (b ⫽ 4.11, SE ⫽ .97, p ⬍ .001)
groups also showed significant growth in their use of behavioral
strategies as measured by SFS scores, with the increase being
significantly larger in the ACCESS condition, Wald (1) ⫽ 42.24,
p ⬍ .001, d ⫽ .81 [.56, 1.07]. Analyses of maladaptive thinking as
measured by ACS-CV scores indicated that the DTC group did not
significantly change over time (b ⫽⫺.44, SE ⫽ .63, p ⫽ .487).
The ACCESS condition did change significantly over time
(b ⫽⫺4.24, SE ⫽ .74, p ⬍ .001), and this decline in maladaptive
thinking was significantly greater for the immediate ACCESS
participants, Wald (1) ⫽ 15.57, p ⬍ .001, d ⫽ .50 [.25, .75]. As
shown in Figure S4 (in the online supplemental materials), these
improvements in clinical change mechanisms were evident at the
end of the active phase and remained stable throughout the main-
tenance phase of ACCESS.
Service Utilization
A descriptive summary of participants’ use of treatment and
other support services appears in Table 3. Because these outcomes
are categorical, scored 0 and 1, an alternate model specification
was used. Growth curve models with categorical indicators do not
afford the same markers of model fit and estimating a multiple-
group model is much less straightforward for categorical out-
comes. As before, latent intercept (1, 1, 1) and slope (0,
ⴱ
,1)
factors were estimated, and the residual variances and covariance
for the intercept and slope were freely estimated. Treatment con-
dition was included as an observed predictor (coded 0 ⫽ delayed,
1 ⫽ immediate). This model thus estimates the overall slope for
the entire sample, along with how treatment status predicts varia-
tion in the slope.
The sample overall did not change in its use of disability service
accommodations over time, b ⫽ .39, SE ⫽ .49, p ⫽ .415, but
treatment status significantly moderated change, with the imme-
diate ACCESS condition showing a significant increase in using
disability services, b ⫽ 1.96, SE ⫽ .58, p ⫽ .001, d ⫽ 1.03 [.48,
1.59]. Although the sample overall increased its use of ADHD
medication, b ⫽ 3.16, SE ⫽ 1.39, p ⫽ .022, treatment status did
not significantly moderate this change, b ⫽⫺.81, SE ⫽ 1.24, p ⫽
.513, d ⫽ .18 [⫺.32, .68]. There was no change in overall sample
use of medications for other medical and mental health conditions,
b ⫽ 1.36, SE ⫽ 12.00, p ⫽ .910, and treatment status did not
significantly moderate the slope, b ⫽⫺.58, SE ⫽ 1.75, p ⫽ .740,
d ⫽ .25 [⫺1.02, 1.52]. Likewise, the sample overall did not change
in its use of counseling services delivered outside of ACCESS,
b ⫽⫺.20, SE ⫽ .28, p ⫽ .468, and treatment status did not
significantly moderate the slope, b ⫽⫺.03, SE ⫽ .20, p ⫽ .900,
d
⫽ .13 [⫺1.40, 1.66].
Clinical Significance of Findings
To inform clinical practice, reliable change indices (RCI; Ja-
cobson & Truax, 1992) were calculated to determine individual
rates of response to treatment. Preactive to postmaintenance phase
difference scores were used for these calculations, with positive
differences reflecting desired therapeutic change for all outcome
measures. Consistent with the Jacobson and Truax (1992) guide-
lines, RCIs greater than 1.96 represented evidence of statistically
significant improvement. Although positive RCIs ⱕ1.96 can re-
flect improvement, these changes are not of a magnitude to be
considered statistically significant and therefore are likely due to
chance. Because individuals with ADHD are at increased risk for
displaying deterioration in their functioning (Barkley, 2015), a
third clinical significance category was generated, operationally
defined as RCIs ⬍0, to examine outcomes reflecting a worsening
in functioning over time.
Higher rates of reliable improvement among immediate
ACCESS participants were revealed by
2
analyses of the ob-
Table 3
Service Utilization by Group Over Time
Service % Preactive % Postactive % Postmaintenance
Disability services
ACCESS 25.3 67.3 60.9
DTC 22.1 37.5 38.0
ADHD medication
ACCESS 53.3 68.9 67.0
DTC 41.7 59.4 71.9
Other medication
ACCESS 26.1 24.0 30.1
DTC 29.1 32.4 37.6
Counseling services
ACCESS 33.7 25.3 34.5
DTC 52.4 39.4 45.1
Note. Disability services ⫽ use of formal disability accommodations
approved by campus disability office; ACCESS ⫽ immediate treatment;
DTC ⫽ Delayed Treatment Control; ADHD ⫽ attention deficit/
hyperactivity disorder; ADHD medication ⫽ use of medication to treat
ADHD; Other medication ⫽ use of medication to treat other mental health
and medical conditions; Counseling services ⫽ use of counseling received
outside of ACCESS program.
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
29
CBT FOR COLLEGE STUDENTS WITH ADHD
served RCI distributions (see Table 4), in terms of inattention (61.3
vs. 31.4%), EF (50.5 vs. 30.0%), anxiety (10.6 vs. 2.0%), knowl-
edge of ADHD (43.6 vs. 8.8%), and use of behavioral strategies
(31.2 vs. 10.2%). Although rates of reliable improvement were
essentially equivalent for immediate ACCESS and DTC partici-
pants with respect to depression and maladaptive thinking patterns,
higher percentages of DTC participants displayed a worsening in
their reports of both depression (54.4 vs. 37.9%) and maladaptive
thinking (41.7 vs. 23.2%). Further evidence of this increased risk
for a deterioration in functioning among DTC versus immediate
ACCESS participants was also seen among the distributions for
inattention (22.5 vs. 12.9%), EF (40.0 vs. 22.6%), anxiety (52.0 vs.
42.6%), knowledge of ADHD (22.5 vs. 5.3%), and behavioral
strategy use (27.6 vs. 9.7%).
Discussion
Findings from this large-scale multisite RCT revealed numerous
improvements in functioning among the college students with
ADHD who received ACCESS on an immediate versus delayed
basis. In terms of primary outcomes, immediate ACCESS partic-
ipants displayed statistically significant greater declines in their
overall ADHD symptomatology, which was driven largely by a
decline in their self-reported inattention symptoms. Effect sizes
associated with these differences were medium in strength (Co-
hen’s d ranging from .39 to .50). Immediate ACCESS participants
also displayed statistically significant improvements in executive
functioning (EF), with medium effect sizes noted for overall EF
deficits (d ⫽ .56), as well as for EF deficits pertaining specifically
to behavioral regulation (d ⫽ .43) and metacognition (d ⫽ .43)
skills. Contrary to study expectations, neither group exhibited a
statistically significant decline in overall levels of depression.
Although immediate ACCESS participants did not show a signif-
icant decline in overall levels of anxiety, there was a significant
increase in anxiety for the DTC group. The slopes between the two
groups were significantly different, thus suggesting a significant
worsening of anxiety symptoms among DTC participants.
Examination of hypothesized mechanisms of clinical change
and participant service utilization also revealed statistically signif-
icant differences between the groups. Although both groups
showed increases over time in their knowledge of ADHD and use
of behavioral strategies, these increases were significantly greater
for participants in the immediate ACCESS group versus the DTC
condition. Effect sizes associated with these group differences
were large, with Cohen’s d estimates of 1.21 and .81 for ADHD
knowledge and behavioral strategies, respectively. The immediate
ACCESS group also displayed a significantly greater decline in
maladaptive thinking than the DTC condition, with the difference
between the groups being of moderate effect size (d ⫽ .50). Such
improvements in ADHD knowledge, use of behavioral strategies,
and adaptive thinking skills, as measured by our study-specific
measures, speak to their potential role as clinical change mecha-
nisms, lending support to the construct validity of our design. In
terms of service utilization, group status moderated use of disabil-
ity services, with immediate ACCESS participants displaying a
significant increase in their use of disability accommodations.
Both groups exhibited significantly increased use of ADHD med-
ications over time, but this increase was not moderated by group
status. The fact that both groups increased their use of ADHD
medication may have been facilitated by participants’ receipt of
written screening evaluation summaries that could be used as
documentation for receiving such services. Neither group, how-
ever, displayed statistically significant increases in their use of
medication for other mental health conditions or in their partici-
pation in counseling outside of ACCESS.
Our clinical significance analyses, which address therapeutic
change at the level of individuals rather than group aggregates,
also revealed findings in line with study expectations. Relative to
DTC participants, higher percentages of immediate ACCESS par-
ticipants displayed reliable improvements in multiple domains of
functioning, including self-reported inattention symptoms, execu-
tive functioning, anxiety symptoms, knowledge of ADHD, and use
of behavioral strategies. Of additional clinical significance are
findings at the other end of the continuum. Specifically, higher
percentages of DTC participants displayed a worsening in their
functioning relative to immediate ACCESS participants in terms of
inattention, executive functioning, depression, anxiety, knowledge
of ADHD, behavioral strategy use, and maladaptive thinking. Such
evidence of a deterioration in functioning is not completely unex-
pected, given what is known about the deleterious impact of
ADHD across the life span (Barkley, 2015). What is surprising,
and at the same time sobering, is the magnitude of the worsening
and the fact that it occurred within a relatively short 12-month time
frame among DTC participants who could and did receive treat-
ments other than ACCESS (e.g., ADHD medication).
Although it is clinically meaningful that ACCESS participants
were less likely to experience a worsening in their depression and
Table 4
Treatment Response Classifications Based on Reliable
Change Indices
Outcome % Worse % Improved
% Reliable
improvement
2
CAARS IN
ACCESS 12.9 25.8 61.3 17.55
ⴱⴱⴱ
DTC 22.5 46.1 31.4
BRIEF-A GEC
ACCESS 22.6 26.9 50.5 9.89
ⴱⴱ
DTC 40.0 30.0 30.0
BDI-II Total
ACCESS 37.9 41.1 21.1 6.22
ⴱ
DTC 54.4 26.2 19.4
BAI Total
ACCESS 42.6 46.8 10.6 6.93
ⴱ
DTC 52.0 46.1 2.0
TOAK Total
ACCESS 5.3 51.1 43.6 35.89
ⴱⴱⴱ
DTC 22.5 68.6 8.8
SFS Total
ACCESS 9.7 58.1 31.2 18.45
ⴱⴱⴱ
DTC 27.6 62.2 10.2
ACS-CV Total
ACCESS 23.2 65.3 11.6 8.07
ⴱ
DTC 41.7 51.5 6.8
Note. CAARS IN ⫽ Conners Adult ADHD Rating Scale Inattention;
DTC ⫽ Delayed Treatment Control; BRIEF-A GEC ⫽ Behavioral Rating
Inventory of Executive Functioning–Adults Global Executive Composite;
BDI-II ⫽ Beck Depression Inventory; BAI ⫽ Beck Anxiety Inventory;
TOAK ⫽ Test of ADHD Knowledge; SFS ⫽ Strategies for Success;
ACS-CV ⫽ ADHD Cognitions Scale–College Version.
ⴱ
p ⬍ .05.
ⴱⴱ
p ⬍ .01.
ⴱⴱⴱ
p ⬍ .001.
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
30
ANASTOPOULOS, LANGBERG, EDDY, SILVIA, AND LABBAN
anxiety symptoms according to the RCI results, their failure to
improve in these domains was somewhat surprising. This lack of
improvement could be due to the timing of when the adaptive
thinking portion of ACCESS directly addresses emotional func-
tioning. Because this occurs in Week 5 of the 8-week active phase
(see Figure 1), ACCESS participants may not have had enough
time to master the adaptive thinking skills necessary for bringing
about improvements in depression and anxiety. Assuming this to
be the case, one option for addressing this would be to identify
participants with elevated pretreatment levels of depression/anxi-
ety and to have mentors begin targeting these emotional features at
an earlier stage of ACCESS. Mentors could also encourage de-
pressed/anxious participants to seek out and concurrently receive
more intensive individual CBT counseling outside of ACCESS.
Such recommendations are in keeping with the notion that ADHD
is best managed via multimodal interventions (Barkley, 2015). In
this regard, ACCESS is well suited to being used in combination
with other treatments (e.g., medication, accommodations, counsel-
ing) to address the multiple psychosocial needs of emerging adults
with ADHD attending college.
Despite the encouraging nature of the obtained findings, it
remains necessary to acknowledge limitations that have bearing on
conclusions drawn from this RCT. For example, the primary and
secondary outcome measures reported in this article were some-
what limited in scope and based exclusively on self-report. As
noted earlier, our RCT did include measures examining other
outcomes (e.g., academic, general daily functioning) but space
limitations precluded their inclusion in the current article. These
will be addressed subsequently, including analyses of more objec-
tive measures of academic functioning drawn from educational
records (see Appendix). Two additional issues not addressed in
this article are: (a) the temporal stability of treatment-induced
improvements following termination from ACCESS, and (b) the
potential moderating effects of sex/gender, race/ethnicity, and
variables of clinical interest (e.g., comorbid features) on response
to treatment. Both issues will be thoroughly examined in a subse-
quent article focused on the treatment response of immediate
ACCESS participants, for whom outcome data are available not
only from the active and maintenance phases, but also from a
follow-up assessment (see Figure 2) conducted 6 months after
participation in ACCESS had been completed. The fact that im-
mediate and delayed treatment participants could receive other
forms of treatment while participating in the study makes it diffi-
cult to ascertain the unique contribution that ACCESS made to
observed improvements in outcome. Evidence indirectly suggest-
ing that ACCESS did indeed contribute to treatment gains may be
inferred from the absence of group differences in their use of other
treatments (i.e., ADHD medication, medication for other mental
health conditions, counseling services). Another potential limita-
tion affecting the external validity of these findings is the gender
distribution of our sample (66% female), which differs from the
relatively higher proportion of males known to have ADHD in the
general population. The reasons for this discrepancy are not en-
tirely clear, but it is first important to note that the gender distri-
bution of our sample is in line with the 60 – 67% representation of
female undergraduates at our two sites. Also speaking to this issue
is the fact that longitudinal research has shown that females with
ADHD generally attain more years of formal education than do
males with this same condition (Barkley et al., 2008).
Bearing these limitations in mind, findings from this large
multisite RCT study build upon those reported from our earlier
open clinical trial (Anastopoulos & King, 2015; Anastopoulos et
al., 2018) and provide strong evidence in support of the efficacy of
ACCESS as a treatment for emerging adults with ADHD attending
college. Although ACCESS shares features found in other psycho-
social treatments for college students with ADHD (e.g., CBT,
OTMP, coaching), it uniquely blends many of these components
together into a single treatment package that is further enhanced by
the inclusion of novel treatment elements, such as: an intensive
ADHD knowledge component to give college students a develop-
mentally appropriate understanding of their own ADHD; simulta-
neous delivery of group treatment and individual mentoring to
facilitate acquisition and mastery of new knowledge and skills; and
a longer duration of treatment (i.e., active and maintenance phases
delivered across two semesters) to better address the chronic
nature of ADHD. Given the clinically challenging nature of the
college students in the study and the rigor with which ADHD and
comorbid conditions were identified in our multisite sample, it is
likely that ACCESS is well-suited to addressing the needs of other
students with ADHD in postsecondary settings. Its feasibility as a
treatment option stems in part from a consideration of the fact that
participation in ACCESS was quite high during the active treat-
ment phase: 83.2% attended at least six of eight planned group
sessions; 85.7% attended a comparable number of mentoring ses-
sions. Also speaking to its feasibility is that ACCESS was imple-
mented in two different university settings with the strong support
of campus support staff. Thus, our findings represent an important
first step in closing the gap from research to practice. Left to future
research is the task of determining how effectively ACCESS can
be disseminated in other college settings, especially those in which
resources (e.g., disability services) and staffing (e.g., level of
ADHD expertise) may differ from those of the two sites in the
current study, thereby potentially requiring minor changes in staff
training and program implementation.
In conclusion, college students with ADHD are at increased risk
for a multitude of educational and psychosocial difficulties that
have serious personal, institutional, and public health implications,
not only during college, but also during the transition into a
postcollege world where demands for self-regulation are greater.
To reduce this risk, it is important for college students with ADHD
to have ready access to evidence-based treatment. Building on the
results of our open clinical trial, findings from the current RCT
suggest that ACCESS is a promising new evidence-based treat-
ment that can play an important role in the overall clinical man-
agement of college students with ADHD.
References
American Psychiatric Association. (2013). Diagnostic and statistical man-
ual of mental disorders (5th ed.).
Anastopoulos, A. D., DuPaul, G. J., Weyandt, L. L., Morrissey-Kane, E.,
Sommer, J. L., Rhoads, L. H., Murphy, K. R., Gormley, M. J., &
Gudmundsdottir, B. G. (2018). Rates and patterns of comorbidity among
first-year college students with ADHD. Journal of Clinical Child and
Adolescent Psychology, 47(2), 236 –247. https://doi.org/10.1080/
15374416.2015.1105137
Anastopoulos, A. D., & King, K. A. (2015). A cognitive-behavior therapy
and mentoring program for college students with ADHD. Cognitive and
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
31
CBT FOR COLLEGE STUDENTS WITH ADHD
Behavioral Practice, 22(2), 141–151. https://doi.org/10.1016/j.cbpra
.2014.01.002
Anastopoulos, A. D., King, K. A., Besecker, L. H., O’Rourke, S. R., Bray,
A. C., & Supple, A. J. (2020). Cognitive-behavior therapy for college
students with ADHD: Temporal stability of improvements in function-
ing following active treatment. Journal of Attention Disorders, 24(6),
863– 874. https://doi.org/10.1177/1087054717749932
Antshel, K. M., Hier, B. O., & Barkley, R. A. (2014). Executive function-
ing theory and ADHD. In S. Goldstein & J. A. Naglieri (Eds.), Hand-
book of executive functioning (pp. 107–120). Springer. https://doi.org/
10.1007/978-1-4614-8106-5_7
Arnett, J. J. (2007). Emerging adulthood: What is it, and what is it good
for? Child Development Perspectives, 1(2), 68 –73. https://doi.org/10
.1111/j.1750-8606.2007.00016.x
Barkley, R. A. (2015). Attention-deficit hyperactivity disorder: A handbook
for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A., Murphy, K. R., & Fischer, M. (2008). ADHD in adults:
What the science says. Guilford Press.
Beck, A. T., & Steer, R. A. (1993). Beck Anxiety Inventory manual.
Psychological Corporation.
Beck, A., Steer, R., & Brown, G. (1996). BDI-II, Beck Depression Inven-
tory: Manual (2nd ed.). Psychological Corporation.
Blasé, S. L., Gilbert, A. N., Anastopoulos, A. D., Costello, E. J., Hoyle,
R. H., Swartzwelder, H. S., & Rabiner, D. L. (2009). Self-reported
ADHD and adjustment in college: Cross-sectional and longitudinal
findings. Journal of Attention Disorders, 13(3), 297–309. https://doi.org/
10.1177/1087054709334446
Conners, C. K., Erhardt, D., & Sparrow, E. (2006). Conners’ Adult ADHD
Rating Scales. Multi-Health Systems.
DuPaul, G. J., Franklin, M. K., Pollack, B. L., Stack, K. S., Jaffe, A. R.,
Gormley, M. J., Anastopoulos, A. D., & Weyandt, L. L. (2018). Pre-
dictors and trajectories of educational functioning in college students
with and without ADHD. Journal of Postsecondary Education and
Disability, 31(2), 161–178.
DuPaul, G. J., Power, T. J., Anastopoulos, A. D., & Reid, R. (2016). ADHD
Rating Scale-5 for children and adolescents: Checklists, norms, and
clinical interpretation. Guilford Press.
DuPaul, G. J., Weyandt, L. L., Rossi, J. S., Vilardo, B. A., O’Dell, S.,
Carson, K. M., Verdi, G., & Swentosky, A. (2012). Double-blind,
placebo-controlled, crossover study of the efficacy and safety of lisdex-
amfetamine dimesylate in college students with ADHD. Journal of
Attention Disorders, 16(3), 202–220. https://doi.org/10.1177/
1087054711427299
Eagan, K., Stolzenberg, E. B., Ramirez, J. J., Aragon, M. C., Suchard,
M. R., & Hurtado, S. (2014). The American freshman: National norms
fall 2014. Higher Education Research Institute, UCLA.
Enders, C. K. (2010). Applied missing data analysis. Guilford Press.
First, M. B., Williams, J. B. W., Karg, R. S., & Spitzer, R. L. (2015).
Structured clinical interview for DSM–5–Research version (SCID-5-
RV). American Psychiatric Association.
Fleming, A. P., & McMahon, R. J. (2012). Developmental context and
treatment principles for ADHD among college students. Clinical Child
and Family Psychology Review, 15, 303–329. https://doi.org/10.1007/
s10567-012-0121-z
Fleming, A. P., McMahon, R. J., Moran, L. R., Peterson, A. P., &
Dreessen, A. (2015). Pilot randomized controlled trial of dialectical
behavior therapy group skills training for ADHD among college stu-
dents. Journal of Attention Disorders
, 19(3), 260 –271. https://doi.org/
10.1177/1087054714535951
Gormley, M. J., DuPaul, G. J., Weyandt, L. L., & Anastopoulos, A. D.
(2019). First-year GPA and academic service use among college stu-
dents with and without ADHD. Journal of Attention Disorders, 23(14),
1766 –1779. https://doi.org/10.1177/1087054715623046
Gu, Y., Xu, G., & Zhu, Y. (2018). A randomized controlled trial of
mindfulness-based cognitive therapy for college students with ADHD.
Journal of Attention Disorders, 22(4), 388 –399. https://doi.org/10.1177/
1087054716686183
He, J., & Antshel, K. (2017). Cognitive behavioral therapy for attention
deficit/hyperactivity disorder (ADHD) in college students: A review of
the literature. Cognitive and Behavioral Practice, 24(2), 152–173.
https://doi.org/10.1016/j.cbpra.2016.03.010
Hechtman, L. (2017). Attention deficit hyperactivity disorder: Adult out-
come and its predictors. Oxford University Press.
Jacobson, N. S., & Truax, P. (1992). Clinical significance: A statistical
approach to defining meaningful change in psychotherapy research. In
A. E. Kazdin (Ed.), Methodological issues & strategies in clinical
research (pp. 631– 648). American Psychological Association. https://
doi.org/10.1037/10109-042
Knouse, L. E., Mitchell, J. T., Kimbrel, N. A., & Anastopoulos, A. D.
(2019). Development and evaluation of the ADHD Cognitions Scale for
adults. Journal of Attention Disorders, 23(10), 1090–1100. https://doi
.org/10.1177/1087054717707580
LaCount, P. A., Hartung, C. M., Shelton, C. R., Clapp, J. D., & Clapp,
T. K. (2015). Preliminary evaluation of a combined group and individual
treatment for college students with attention-deficit/hyperactivity disor-
der. Cognitive and Behavioral Practice, 22(2), 152–160. https://doi.org/
10.1016/j.cbpra.2014.07.004
LaCount, P. A., Hartung, C. M., Shelton, C. R., & Stevens, A. E. (2018).
Efficacy of an organizational skills intervention for college students with
ADHD symptomatology and academic difficulties. Journal of Attention
Disorders, 22(4), 356 –367. https://doi.org/10.1177/1087054715594423
Lewandowski, L., Gathje, R. A., Lovett, B. J., & Gordon, M. (2013).
Test-taking skills in college students with and without ADHD. Journal
of Psychoeducational Assessment, 31(1), 41–52. https://doi.org/10.1177/
0734282912446304
Meaux, J. B., Green, A., & Broussard, L. (2009). ADHD in the college
student: A block in the road. Journal of Psychiatric and Mental Health
Nursing, 16(3), 248 –256. https://doi.org/10.1111/j.1365-2850.2008
.01349.x
Miller, L. A., Lewandowski, L. J., & Antshel, K. M. (2015). Effects of
extended time for college students with and without ADHD. Journal of
Attention Disorders, 19(8), 678 – 686. https://doi.org/10.1177/
1087054713483308
Pinho, T. D., Manz, P. H., DuPaul, G. J., Anastopoulos, A. D., & Weyandt,
L. L. (2019). Predictors and moderators of quality of life among college
students with ADHD. Journal of Attention Disorders, 23(14), 1736 –
1745. https://doi.org/10.1177/1087054717734645
Preacher, K. J., Wichman, A. L., MacCallum, R. C., & Briggs, N. E.
(2008). Latent growth curve modeling
. SAGE. https://doi.org/10.4135/
9781412984737
Prevatt, F., & Yelland, S. (2015). An empirical evaluation of ADHD
coaching in college students. Journal of Attention Disorders, 19(8),
666 – 677. https://doi.org/10.1177/1087054713480036
Rabiner, D. L., Anastopoulos, A. D., Costello, E. J., Hoyle, R. H., McCabe,
S. E., & Swartzwelder, H. S. (2009). Misuse and diversion of prescribed
ADHD medications by college students. Journal of Attention Disorders,
13(2), 144 –153. https://doi.org/10.1177/1087054708320414
Ramsay, J. R. (2015). Psychological assessment of adults with ADHD. In
R. A. Barkley (Ed.), Attention-deficit hyperactivity disorder: A hand-
book for diagnosis and treatment (pp. 475–500). Guilford Press.
Roth, R. M., Isquith, P. K., & Gioia, G. A. (2005). Behavior rating
inventory of executive function–Adult version. Psychological Assess-
ment Resources.
Safren, S., Perlman, C., Sprich, S., & Otto, M. W. (2005). Mastering your
adult ADHD: A cognitive behavioral treatment program therapist guide.
Oxford University Press.
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
32
ANASTOPOULOS, LANGBERG, EDDY, SILVIA, AND LABBAN
Scheithauer, M. C., & Kelley, M. L. (2017). Self-monitoring by college students
with ADHD: The impact on academic performance. Journal of Attention
Disorders, 21(12), 1030 –1039. https://doi.org/10.1177/1087054714553050
Solanto, M. V. (2011). Cognitive-behavioral therapy for adult ADHD:
Targeting executive dysfunction. Guilford Press.
Van der Oord, S., Boyer, B. E., Van Dyck, L., Mackay, K. J., De Meyer,
H., & Baeyens, D. (2020). A randomized controlled study of a
cognitive behavioral planning intervention for college students with
ADHD: An effectiveness study in student counseling services in
Flanders. Journal of Attention Disorders, 24(6), 849–862. https://doi
.org/10.1177/1087054718787033
Weyandt, L. L., & DuPaul, G. J. (2012). College students with ADHD:
Current issues and future directions. Springer.
Wolf, L. E., Simkowitz, P., & Carlson, H. (2009). College students with
attention-deficit/hyperactivity disorder. Current Psychiatry Reports, 11,
415– 421. https://doi.org/10.1007/s11920-009-0062-5
Appendix
Data Transparency Statement
The data reported in this article have not been previously pub-
lished but were collected as part of a larger data collection effort
(at one or more points in time). Additional findings from this larger
data set have been reported in a second article currently under
editorial review. Both articles examine the efficacy of the
ACCESS intervention but address conceptually different out-
comes. The current article addresses treatment-induced changes in
primary ADHD symptoms, associated executive functioning and
emotional features (i.e., depression, anxiety), clinical change
mechanisms, and service utilization. The second article focuses
exclusively on functional outcomes, in terms of treatment-induced
changes in both educational functioning (i.e., grade point average,
number of semester credits attempted, self-reported learning and
study strategies) and daily functioning (i.e., general well-being,
daily functioning and performance, relationships and communica-
tion).
Received May 2, 2020
Revision received September 30, 2020
Accepted October 5, 2020 䡲
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
33
CBT FOR COLLEGE STUDENTS WITH ADHD
