A Cognitive-Behavior Therapy and Mentoring Program for College Students With ADHD
By: Arthur D. Anastopoulos and Kristen A. King
Anastopoulos, A.D. & King, K.A. (2015). A cognitive-behavior therapy and mentoring program
for college students with ADHD. Cognitive and Behavioral Practice, 22(2), 141-151. DOI:
10.1016/j.cbpra.2014.01.002
Made available courtesy of Elsevier: https://doi.org/10.1016/j.cbpra.2014.01.002
This work is licensed under a Creative Commons Attribution-
NonCommercial-NoDerivatives 4.0 International License.
Abstract:
College students with ADHD are at increased risk for a number of functional impairments, the
severity of which is of sufficient clinical significance to warrant intervention (DuPaul &
Weyandt, 2009). Very little treatment research of this type has been conducted to date (Green &
Rabiner, 2012). The need for such research is critical, given the increasing numbers of students
with ADHD attending college (Pryor, Hurtado, DeAngelo, Blake, & Tran, 2010), their increased
risk for dropping out of college, and the known negative life outcomes for which they may be at
increased risk later as adults (Barkley, Murphy, & Fischer, 2008). To address this situation we
recently developed and began testing Accessing Campus Connections and Empowering Student
Success (ACCESS). The active phase of ACCESS provides group cognitive behavior therapy
(CBT), accompanied by individual mentoring. Booster group CBT and mentoring sessions are
provided during a maintenance phase. Preliminary findings have revealed significant increases in
ADHD knowledge, use of organizational skills, and reductions in maladaptive thinking, all of
which are presumed mechanisms of clinical change. Such changes have been accompanied by
reductions in ADHD symptoms, improvements in executive functioning, educational benefits,
improved emotional well-being, and increased use of disability services and other campus
resources. Although promising, such findings are limited by the fact that ACCESS has thus far
been tested in an open clinical trial. Thus, additional research is needed to determine its efficacy
and effectiveness.
Keywords: adult ADHD | college students | clinical trial | psychosocial intervention | cognitive-
behavior therapy
Article:
Attention-deficit/hyperactivity disorder (ADHD) is a chronic life-span condition
associated with long-term impairment in educational attainment, occupational status, and social
relationships, as well as increased risk for psychopathology and legal difficulties (Barkley,
Murphy, & Fischer, 2008; Mannuzza, Gittelman-Klein, Bessler, Malloy, & LaPadula, 1993).
Individuals identified as having ADHD in childhood are significantly less likely to graduate from
high school. Significantly fewer (20–21%) go on to college relative to their non-ADHD peers
(68–78%; Barkley et al., 2008).
Although the exact prevalence of individuals with ADHD attending college is not well
established, estimates derived from large sample studies indicate that approximately 2 to 8% of
college students report clinically significant symptoms of ADHD (DuPaul et al., 2001; McKee,
2008; Norvilitis, Ingersoll, Zhang, & Jia, 2008). Consistent with these estimates are the results of
a recently conducted national survey, which revealed that 5% of incoming first-year students
reported having ADHD (Pryor, Hurtado, DeAngelo, Blake, & Tran, 2010). Also, among college
students who receive disability accommodations, approximately 25% receive such services on
the basis of an ADHD diagnosis (Wolf, 2001). Thus, clinically significant ADHD symptoms
would appear to affect a substantial segment of the college population.
As is true for children and adults, the impact of ADHD on the daily and long-term
functioning of college students with ADHD is clinically significant and broad in nature. In terms
of educational functioning, it has been reported that college students with ADHD maintain lower
grade point averages (GPAs), withdraw from a greater number of courses, and take longer to
complete their degree programs relative to control individuals without ADHD (Barkley et al.,
2008). Of additional clinical and public health significance, Barkley and his colleagues (2008)
found that only 9.1% of individuals who display ADHD in young adulthood actually graduate
from college compared to 60.6% of the non-ADHD control group. Impairment in psychological
and social functioning may occur as well, with many studies indicating that college students with
ADHD are more likely to experience higher levels of depression, anxiety, and other types of
psychological distress (e.g., Heiligenstein & Keeling, 1995; Rabiner, Anastopoulos, Costello,
Hoyle, & Swartzwelder, 2008; Weyandt et al., 2003), and to display lower levels of overall
adjustment, social skills, and quality of life (Grenwald-- Mayes, 2002; Shaw-Zirt, Popali-Lehane,
Chaplin, & Bergman, 2005). A handful of studies has explored the driving performance of
college students with ADHD and the results consistently indicate that students with ADHD have
a higher number of driving citations, speeding violations, license suspensions/revocations, and
motor vehicle accidents relative to non-ADHD peers (Barkley, Murphy, DuPaul, & Bush, 2002;
Richards, Deffenbacher, & Rosén, 2002). Preliminary findings also suggest that college students
with ADHD may be at higher risk for substance abuse relative to non-ADHD controls (Kollins,
2008; Upadhyaya et al., 2005).
Conceptual Model for Understanding Impairment
The degree to which college students with ADHD experience impairment may seem
counterintuitive at some level, given that such individuals possessed the qualifications necessary
to be admitted to college (Glutting, Youngstrom, & Watkins, 2005). Some researchers have
speculated that inadequate educational coping strategies, poor organizational and study skills,
and inefficient time management may underlie these difficulties (e.g., Heiligenstein, Guenther,
Levy, Savino, & Fulwiler, 1999; Norwalk, Norvilitis, & MacLean, 2008; Reaser, Prevatt,
Petscher, & Proctor, 2007; Weyandt et al., 2003). Yet another possible explanation stems from a
theoretical consideration of what could be termed a “perfect storm” of circumstances that
converge upon students with ADHD as they enter college. Prior to college, many supports may
be in place to help manage the deficits in self-regulation (Barkley, 2006) that a student with
ADHD might display. Such supports might include, for example, an individualized educational
plan or 504 accommodations in school, regular use of pharmacotherapy to address school--
related ADHD difficulties, and parental monitoring of school work loads, upcoming tests, and
assignment due dates. Parental supervision may also extend into nonacademic domains, thereby
relieving the student of the responsibility of managing finances, daily schedules, and other
personal matters. As is true for any student, demands for self-regulation skyrocket upon entering
college, not only with respect to educational matters but also in terms of various personal and
social responsibilities. This developmental transition is indeed normative and often the reason
that beginning students experience trouble adjusting to college life. For students with ADHD,
however, this same developmental challenge is amplified many times over due to their inherent
deficit in self-regulation (Fleming & McMahon, 2012), and the fact that most, if not all, external
supports have been removed (Meaux, Green, & Broussard, 2009). Further complicating matters
is that many students do not fully understand or accept their ADHD, and therefore are reluctant
to seek campus support services that require disclosure of a condition that makes them different
from their peers.
Treatment of ADHD in College
While additional research is needed to identify the causal mechanisms responsible for
these outcomes, what remains clear is that college students with ADHD are at increased risk for
a broad range of functional impairments and that the severity of these impairments is of
sufficient clinical significance to warrant intervention. Somewhat surprisingly, very little
treatment research of this type has been conducted to date (DuPaul & Weyandt, 2009; Green &
Rabiner, 2012). The only medication study of which we are aware is one recently conducted by
DuPaul and his colleagues (2012), who utilized a double-blind, placebo-- controlled crossover
design to investigate the efficacy and safety of Lisdexamfetamine dimesylate (LDX) among
college students with ADHD. Their findings led them to conclude that LDX was efficacious,
bringing about large reductions in ADHD symptoms and improvements in executive functioning,
along with smaller effects for psychosocial functioning. In terms of studies using nonmedication
approaches, improvements in educational functioning have been reported for college students
with ADHD following exposure to semester-long strategy instruction (e.g., organization, test
taking, note taking) delivered by graduate students in special education (Allsop, Minskoff &
Bolt, 2005). Of note, one of the factors thought to be related to successful outcome in this study
was the supportive nature of the strategy instructor–student relationship, which was derived from
qualitative analyses. Less compelling but positive outcome findings have also been reported in
studies that used coaching (Prevatt, Lampropoulos, Bowles, & Garrett, 2011) and assistive
reading software (Hecker, Burns, Elkind, Elkind, & Katz, 2002) to address the needs of college
students with ADHD.
A New Treatment Approach: ACCESS
To the best of our knowledge, no well-controlled study to date has investigated the
efficacy of psychological treatment of college students with ADHD. As a first step in addressing
this need, our team has been conducting an open clinical trial over the past two years with
college students who have ADHD. Our program, known as ACCESS (Accessing Campus
Connections and Empowering Student Success) is the student support piece of a larger project
known as College STAR (Supporting Transition, Access, and Retention), which is a three-year
foundation
1
-funded project awarded to the University of North Carolina system and currently
involving the University of North Carolina at Greensboro (UNCG), East Carolina University,
and Appalachian State University.
Over the past two years numerous refinements have been made to ACCESS, some of
which impacted its duration. For example, in its first semester of operation ACCESS began as a
six-week pilot program for the first six participants. In the two semesters that followed, a total of
31 participants received a 10-week version of this same program. It soon became apparent that
this 10-week program was very difficult to incorporate into a single 15-week semester, given the
need to recruit and screen participants during the first few weeks of the semester and then do
posttreatment measures at the end of the semester. Primarily for this reason ACCESS was
shortened to eight weeks for the other six participants included in this paper. ACCESS has
remained an eight-week program for the new participants enrolled this fall and will remain an
eight-week program for the duration of our three-year funding period. Generally speaking, the
topic content has remained the same regardless of how many sessions were delivered. Although
the 10-session program allowed for covering certain topics in greater detail, whatever benefits
may have resulted from this 10-session format were outweighed by the costs—in this case, the
impracticality of conducting all pretreatment, treatment, and posttreatment aspects of the
program within a single 15-week semester.
In its current and final form, ACCESS now includes an eight-week active treatment
protocol, followed by a maintenance phase in the subsequent semester. In the active treatment
phase participants meet weekly for 90 minutes of group cognitive behavior therapy (CBT) and
also receive eight 30-minute individual mentoring sessions. During the maintenance phase,
participants participate in two booster CBT group sessions scheduled near the start and midpoint
of the semester, and receive five to six 30-minute individual mentoring sessions occurring every
two to three weeks.
Group Treatment
In the absence of existing psychosocial treatment studies with college students, we turned
to the adult ADHD treatment literature to help guide the creation of the ACCESS group
treatment protocol. In particular, we were influenced by the seminal empirical work of Safren
(Safren, Perlman, Sprich, & Otto, 2005) and Solanto (2011). Thus, evident in the group treatment
portion of our protocol are CBT elements common to both programs, which we have adapted for
use with college students and standardized in a treatment manual. This includes psychoeducation
and skills training to help students cope more effectively with the executive functioning deficits
inherent in ADHD, thereby increasing the likelihood for improving functioning across multiple
life domains. Specifically, ACCESS is designed to increase knowledge of ADHD and awareness
of campus resources; to improve organization, time management, and other behavioral skills; and
to teach cognitive therapy strategies for the purpose of increasing adaptive thinking that
promotes greater treatment adherence and reduced risk for secondary emotional and social
problems.
In contrast with the adult CBT interventions (Safren et al., 2005; Solanto, 2011) that
deliver their main treatment components primarily in a sequential fashion—that is, an ADHD
knowledge module followed by a behavioral skills module followed by a cognitive therapy
module— ACCESS delivers its main treatment components concurrently. More specifically, a
portion of each group treatment session addresses ADHD knowledge, behavioral skills, and
cognitive therapy.
The rationale for doing so was based in part on developmental considerations gleaned
primarily from clinical experience. For many college students, their understanding of ADHD is
limited, often based on what parents and teachers have told them. For still others, their
acceptance and ownership of ADHD is also limited, sometimes due to long-standing
developmentally appropriate resistance to whatever parents and other adults tell them; at other
times, due to a preference not to embrace a label that can have negative connotations, especially
as it relates to acceptance within a peer group. For developmental reasons such as these, along
with preliminary data from our ongoing projects, we concluded that the need for providing
psychoeducation about ADHD was much greater than that for older adults. Thus, we increased
the intensity of the ADHD psychoeducation in the CBT group protocol.
A major reason for simultaneously addressing all three major treatment components in
each CBT group session was to increase the variety of the material being presented in an effort to
maintain student interest and participation in the program. For some students, for example, there
is more need for the cognitive therapy piece than the behavioral piece, or vice versa. Rather than
require students to wait for what they need, potentially boring them and losing their interest
along the way, we opted to present all three treatment components together in each session.
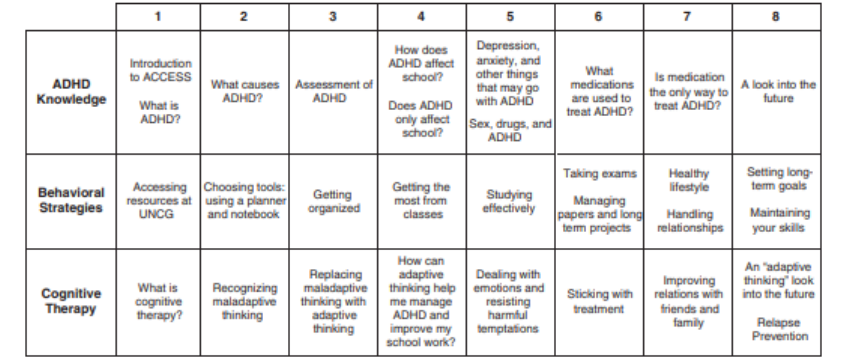
As can be seen in Figure 1, another distinctive feature of ACCESS is that delivery of its
three major components is tailored to be developmentally appropriate for college students.
Moreover, within most sessions the three major components are integrated to address the same or
very similar topics. Portions of several sessions are also set aside for guest speakers to provide
information and to answer questions about the campus support units (e.g., Office of Disabilities
Services [ODS], Counseling Center) they represent.
Figure 1. Session-by-Session Outline for Group Cognitive-Behavior Therapy Component of
ACCESS
Groups generally include three to seven students at multiple points in their undergraduate
education. This group composition encourages the more experienced students to share their
experiences and tips with the less experienced students. While keeping the personal information
discussed in group confidential is emphasized, students are encouraged to support one another
outside of the group (e.g., studying together, helping one another with transportation to the
group). All groups are led by licensed Ph.D.-level psychologists.
At the beginning of every session each group member receives detailed handouts
summarizing the major points of that session. Such handouts provide an additional sensory
modality for processing the session, as well as a template for organizing written notes. These
same handouts also serve to guide between-session practice and later can be used as a reminder
during the maintenance phase and beyond. Students are given a folder to store their handouts and
are encouraged to keep them for later reference.
Although some group content is presented in a lecture format, a back-and-forth, question-
and-answer presentation style is used whenever possible to encourage active student
participation. For example, when discussing how ADHD may affect students academically,
students are invited to share their own perspectives on how ADHD has influenced their academic
functioning. Invariably, stories told by one student spark an immediate “That happened to me
too” from other students who then share their war stories with one another, thereby contributing
to group cohesion. During the behavioral strategies portion of each session, the group leader
often opens the discussion by asking students what strategies are working well, or not so well.
When a participant reports not having success with a particular strategy, the group leader often
asks the other members of the group to give that participant direct feedback, emphasizing what
he or she can do to use a particular strategy more effectively. A common example of this type
of situation is when students show their planners to other group members, pointing out how their
adaptations of the system (e.g., use of different colored pens, blocking out study times in various
ways, stapling “to-do” lists directly into their planners) might also be of benefit to them. Similar
strategies are used during the cognitive therapy portion of treatment, during which a whiteboard
is used as a visual aid to guide students through thought exercises (e.g., completing thought
records challenging maladaptive thoughts).
In contrast with the CBT groups in the active phase of treatment, the two CBT group
sessions in the maintenance phase of treatment are substantially less structured in order to be
tailored to the needs of each participant. In particular, the two scheduled booster sessions provide
an opportunity for addressing new questions about ADHD that may have arisen, for
troubleshooting participants' implementation of behavioral strategies, and for refining participant
use of cognitive therapy strategies. Another important clinical benefit of these booster sessions is
that they provide an opportunity for group members to reconnect with one another and to receive
support from fellow group members.
Mentoring
Concurrent with their group work, students work individually with mentors to help them
apply what they have learned in group, connect with campus resources, and deal with daily life
issues. More specifically, mentors monitor student understanding of ADHD and help them apply
behavioral and adaptive thinking strategies to situations that may occur outside of group
treatment or perhaps are better suited to one-on-one rather than group discussions. As a way of
addressing academic performance and personal success, mentors also provide guidance on how
to access campus support units appropriate to student needs. In addition, mentors help students
develop realistic goals, monitor their follow-through on achieving those goals, and provide
students with ongoing support (Allsop et al., 2005) and personal coaching (Prevatt et al., 2011).
All mentors have a background in psychology, ranging in experience from graduate students in
nonclinical master’s degree programs to postdoctoral fellows in clinical psychology.
During the first session, which occurs during the first week of group CBT, mentors
review students' current academic and personal functioning, use of campus resources, challenges,
and goals for treatment. In subsequent sessions, which run concurrently with the remaining seven
weeks of group CBT, mentors perform a brief check-in with the participant, collaborate with the
participant to set an agenda, review homework from the previous session, review group
materials, set new goals and homework assignments, and cover other topics as needed and as
requested by participants. The time spent on each of these areas varies according to the needs
and interests of each student; applying the material presented in group that the mentor and
student feel would be most helpful is emphasized. In the final session, mentors discuss ways for
students to maintain their skills and performance once treatment ends.
During the maintenance phase, mentoring sessions are less numerous and even more
flexible, guided primarily by student needs and preferences. Thus, some students may choose to
use these sessions to review and refine their use of behavioral strategies, whereas others may opt
for using these sessions primarily for personal goal setting and support.
Method
Participants
Over the past two years a total of 43 undergraduate students from UNCG have formerly
participated in our open clinical trial with ACCESS. Participants were recruited from multiple
sources, including cases seen at a campus-based ADHD specialty clinic where CBT was one of
the recommendations made during a clinical evaluation feedback session (40%); referrals from
the Office of Disability Services (ODS) and other campus units (30%); freshmen who became
aware of the program during summer orientation sessions (19%); students referred by their
parents (5%); and students who learned of the program via word of mouth (6%). Participants
included 27 females and 16 males, encompassing first-- year students through seniors. Ages
ranged from 17 to 27; the mean age of participants is 20.3 years. In line with UNCG
demographics, 16% of the sample is Hispanic, and 21% come from African American and
multiracial backgrounds.
Ninety-five percent of the participants had been diagnosed with ADHD prior to entering
ACCESS; of these, only 53% had been formally diagnosed during childhood or adolescence.
ADHD status was further assessed to ensure that all participants met full DSM-IV criteria for
ADHD as determined either by a recently completed psychological evaluation or by a screening
completed by the ACCESS team. Multiple methods and multiple informants were used to make
this diagnostic determination, consistent with best-practice recommendations for diagnosing
ADHD in adults (Barkley et al., 2008). This included self-report and other report versions of the
ADHD Rating Scale (ADHD RS; DuPaul, Power, Anastopoulos, & Reid, 1998), modified to
address both childhood and current symptoms. Students also completed the Conners Adult
ADHD Rating Scale, Self-Report, Long Version (CAARS-S:L; Conners, Erhardt, & Sparrow,
2006), from which the CAARS-S:L DSM-IV Inattention and Hyperactivity–Impulsivity scores
were used to address the developmental deviance of ADHD symptoms. Together with these
rating scales, a semistructured, clinician-administered interview was conducted to confirm
ADHD status.
Based on student responses to probe questions during a review of background
information, selected modules from the Structured Clinical Interview for DSM Disorders (SCID-
I; First, Spitzer, Gibbon, & Williams, 1996) were administered to evaluate for the presence of
both exclusionary and comorbid psychiatric conditions. Seventeen of the 43 students (40%) met
DSM-IV criteria for mood disorders, and 14 (33%) met DSM-IV criteria for an anxiety disorder.
Other comorbid diagnoses included adjustment disorders, substance abuse and dependence
disorders, and learning disorders. Overall, 25 of the 43 students (58%) had at least one comorbid
diagnosis. A majority of students (59%) reported that, at some point during college, they had
taken psychiatric medication, either for ADHD symptoms or for another disorder. Data also
indicated that 38% of students had utilized psychotherapy since starting college.
Given the high rates of comorbidity reported for adults with ADHD (80%; Barkley et al.,
2008), participants were included in ACCESS even if they had diagnosable depression and
anxiety disorders, which represent the majority of comorbid conditions that are likely to be
present. The comorbid presence of several other conditions, however, was exclusionary,
including autism spectrum disorders, bipolar disorder, and other psychiatric conditions whose
treatment precludes participation in the study. Whether or not they had comorbid diagnoses,
participants receiving pharmacotherapy, psychotherapy, and other types of support services were
allowed into the study, as one of the goals of ACCESS is to increase access to and utilization of
such treatment services.
Measures
Pretreatment data were collected during the two weeks prior to the start of the CBT
groups. Posttreatment data were collected at the end of the final group session. Posttreatment
measures were administered by members of the research team unaffiliated with the participants.
Whenever possible, pretreatment measures were also administered by members of the research
team unaffiliated with the participant; occasionally, the group leader administered pretreatment
measures due to schedule conflicts.
Clinical Change Mechanisms
The underlying assumption of the ACCESS program is that if intended changes occur
with respect to ADHD knowledge, behavioral strategies, and cognitive therapy skills, then
corresponding improvements should occur in the various domains of daily functioning. As a
check on these hypothesized mechanisms of clinical change, four measures have been
administered prior to and immediately following active treatment. The first of these is a 50-item
Test of ADHD Knowledge that we developed, which requires participants to read a stem
description and then respond with either “agree,” “disagree,” or “not sure.” To assess for changes
in use of organization, time management, and other behavioral strategies, we also developed the
Strategies for Success measure, which includes 30 items that students rate on a scale from 1 (not
well) to 5 (very well) regarding how well they perform various behaviors, such as “Using a
planning calendar” and “Setting long-term goals.” Two additional measures were developed to
assess ADHD-related cognitions. The first of these is the ADHD Cognitions Test (ACT), a rating
scale procedure that asks respondents to indicate on a 1 to 5 basis the degree to which they
engage in various ADHD-related cognitions, including items that represent maladaptive
cognitions (e.g., “I need it now,” “Being impulsive is a big part of who I am”), as well as items
that are reverse coded and represent adaptive thinking, such as “I’m careful in making
decisions.” Also developed and implemented as a measure of cognitions was the Cognitive
Response Test for ADHD (CRT-A), which requires respondents to complete sentence stems that
trigger maladaptive thinking responses among college students with ADHD (e.g., “Our professor
gives back our tests and my grade is one of the lowest in the class. I think to myself . . ”; “One of
my friends tells me that he or she will call me back in a few minutes but never does. I think to
myself . . .”). All responses were coded by multiple raters for reliability and given scores of 0 if
they showed no maladaptive thinking patterns, 1 if they showed a maladaptive thinking pattern
that the participant then corrected (e.g., an overgeneralization followed by a retraction of that
statement), or 2 if they showed a maladaptive thinking pattern and no sign that the pattern was
corrected.
Functional Outcome Measures
The CAARS-S:L DSM-IV inattentive symptoms, DSM-IV hyperactive–impulsive
symptoms, and DSM-IV ADHD symptoms total scores were used to assess treatment-induced
changes in primary ADHD symptoms. Working memory and other aspects of executive
functioning were assessed using the Behavior Rating Inventory of Executive Function–Adult
Version (BRIEF-A; Gioia, Isquith, Guy, & Kenworthy, 2000). The BRIEF-A is a self-report
instrument that takes approximately 10 minutes to complete and has adequate psychometric
properties. The BRIEF-A generates three general composite scores—Behavior Regulation Index,
Metacognition Index, and General Executive Composite—all of which served as outcome
variables. Participants also completed dimensional measures of psychological functioning,
including the Beck Depression Inventory–II (Beck, Steer, & Brown, 1996), and the Beck
Anxiety Inventory (Beck & Steer, 1993). Both of these measures have sound psychometric
properties and were used to monitor treatment-induced changes in psychological functioning. As
noted above, one of the goals of ACCESS is to increase participants’ awareness and use of
campus supports and other resources. Thus, students provided responses to service use
questionnaires to determine whether this type of change had taken place. Archival educational
data were also collected, including GPA for each semester, the proportion of course credits
attempted and earned, the number of course withdrawals and incomplete courses, leaves of
absence, and academic probations and suspensions.
Preliminary Findings
Attrition
Only three out of these 43 participants completely dropped out of treatment. Such a low
rate of attrition is in large part due to the high degree of satisfaction with the program, with
100% of the participants who completed posttreatment interviews (N = 30) stating that they
would recommend ACCESS to other students with ADHD. This same level of satisfaction
presumably contributed to the large number of sessions that were attended. Using an 80%
attendance threshold, 86% of our participants finished the CBT group treatment and 84%
completed the mentoring portion. Some participants who were partial completers or who
dropped out of treatment were nonetheless willing to complete posttreatment outcome measures,
and therefore a higher rate of posttreatment data completion (93%) was possible. During the
follow-up semester, 68% of participants attended at least one booster session and 82% met with
their mentor at least once. Full utilization of the program was less common; only 54% attended
both booster sessions and only 54% met with their mentor for five or more sessions.
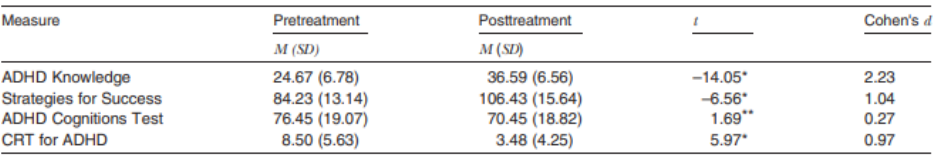
Table 1 Summary of Measures Assessing Clinical Change Mechanisms
Note. ADHD Knowledge = Test of ADHD Knowledge; CRT for ADHD = Cognitive Response
Test for ADHD.
* p ≤ .001; ⁎⁎ p < .10.
Treatment Fidelity
Treatment manuals with detailed session-by-session outlines were developed to guide the
group CBT leaders and mentors in their delivery of the ACCESS program. All CBT group
sessions were video recorded but it was not possible to do so for the mentoring sessions due to
space and equipment limitations. A random sampling and review of the CBT group sessions
revealed excellent adherence to treatment, operationalized in terms of the number of content
items in each session outline that were covered. All reviewed sessions exceeded the 90%
threshold that was used to classify treatment delivery as satisfactory.
Clinical Change Mechanisms
Preliminary two-tailed paired t test analyses of the pretreatment to posttreatment data
revealed significant improvements in all three hypothesized mechanisms of change. This
includes increased knowledge of ADHD, increased use of organizational and other behavioral
strategies, and reduced levels of maladaptive thinking on the CRT-A, all of which were highly
significant (p < .001) and associated with large to very large effect sizes (see Table 1).
Functional Outcome Measures
As shown in Table 2, paired t test analyses revealed significantly reduced levels of
inattentive symptoms (p < .001) and the ADHD symptom total (p < .001), as well as a trend
toward lower levels of hyperactive–impulsive symptoms (p = .054). The effect sizes associated
with these improvements in inattentive symptoms and the ADHD symptom total fell within the
moderate to large range, whereas there was only a small effect found for the changes in
hyperactivity–impulsivity. Significant improvements (p < .001) were also found for the three
domains of executive functioning measured by the BRIEF-A, all of which represented large
effects. Although not statistically significant, trends were detected with respect to reductions
in levels of anxiety (p = .055) and depression (p = .134), for which the effect sizes were small.
The degree to which the above significant findings
represent normalization of functioning was also addressed via examination of scores falling
above and below a 1.5 standard deviation cut point at pretreatment versus posttreatment. For the
ADHD symptom total, the percentage of participants within 1 standard deviation of the mean
increased from 18% at pretreatment to 40% at posttreatment. This change in overall self-reported
ADHD symptoms was driven primarily by the increase in Inattentive scores (8% vs. 28%) and to
a lesser extent by changes in the Hyperactive–Impulsive scores (53% vs. 68%). For the BRIEF-A
Global Executive Composite, the percentage of participants within 1 standard deviation of the
mean increased from 10% at pretreatment to 50% at posttreatment. Increases were also evident
for the Metacognition Index (8% vs. 45%) and the Behavioral Regulation Index (45% vs. 65%).
Mixed findings emerged from preliminary analyses of the archival educational data,
which in part may be due to the fact that no pretreatment data were available for freshmen and
therefore the sample size was reduced. For those for whom complete educational data were
available (N = 23), there was a statistically nonsignificant change in GPA, increasing from 2.3 in
the semester immediately preceding treatment to 2.5 at the end of the semester in which
treatment was provided. A different picture emerged when examining these same educational
data categorically, defined in terms of the university’s cut point for academic probation (i.e.,
GPA below 2.0). More specifically, fewer participants fell into the academic probation range in
the semester in which treatment was provided (18.9%) versus the semester immediately prior
to treatment (26.1%).
Student responses to questionnaires (N = 37) also suggested increased utilization of
campus services. Most striking was the increase in the use of the ODS. Although 41% of
participants were registered with ODS at pretreatment, only 19% had actually met with ODS
staff to develop a list of academic accommodations. At posttreatment, 62% of participants had
chosen to register and 57% of participants were using accommodations. In addition, five students
who had not used medication to treat their ADHD symptoms during college were using
medication by posttreatment and one student who had not sought psychotherapy during college
had begun psychotherapy treatment. Six students who had never used tutoring reported using
tutoring services by the end of the program and seven students who had never used the campus
Writing Center reported that they had used this service at least once.
Case Example
Although the above preliminary findings are encouraging, it is important to keep in mind
that these results emanate from group-based statistical analyses and descriptions. Not included in
such reporting is a detailed analysis of the clinical significance of the findings, that is, the
meaning of the results as they relate to student functioning at an individual level. A formal
examination of clinical significance is beyond the scope of this paper; however, as a way of
capturing how ACCESS might impact a college student with ADHD, the following case example
is presented. Important to note is that all identifying data have been removed from this example;
where necessary, some descriptions have been modified slightly to further protect the identity of
the individual.
“Kimberly” entered the ACCESS program as a junior. She was diagnosed with ADHD
during her elementary school years and had taken medication to treat her ADHD symptoms since
that time. She reported some difficulty in the past with anxiety but only met criteria for ADHD,
combined type, at the time of screening. When she started ACCESS, she was already using some
campus resources; she had registered with ODS and had investigated the possibility of tutoring
as well. She expressed enthusiasm about the opportunity to take part in ACCESS.
Kimberly participated actively in the CBT group sessions, attending all but one session.
As a more senior student than some of her fellow group members, she seemed to enjoy sharing
her tips and experiences with the other students. She made at least one friend in the group who
she saw socially outside of the program. In discussions covering knowledge of ADHD, Kimberly
openly shared her experiences. Kimberly was consistently cooperative when new behavioral
strategies were suggested, and she reported trying a number of new strategies for improving her
time management and academic performance. However, she sometimes seemed resistant to
trying new techniques. For example, when discussing strategies for completing papers, she noted
that procrastination had “worked” for her in the past, so it was difficult to encourage her to
change that habit. Kimberly was already using a planner to some extent at the start of the
program, but she was not yet taking full advantage of it. She was not using the planner to break
down tasks into manageable steps or to schedule study sessions; she improved on both of these
skills during the program. During the CBT portion of the groups, Kimberly was easily able to
provide examples of maladaptive thinking. She was skilled at developing alternate, more realistic
thoughts, whether when working her own thought records or when helping a group member
challenge maladaptive thoughts.
Kimberly attended all of her mentoring appointments. She was very motivated and easily
set short- and long-term goals for herself. At the start of the program, she expressed the idea that
her negative study habits could “never” be changed. During the course of the program she
developed more effective study strategies, learned to stick to a study schedule, and learned better
note-taking procedures and test-taking strategies. In addition, she developed better time
awareness with respect to both academics and social life and improved in her use of to-do lists
and in setting reminder alarms. In addition, she developed better awareness of how her thought
patterns affected her social relationships. Kimberly utilized academic accommodations through
the ODS and participated in campus tutoring as well. Academically, her grades improved; her
GPA during her semester of treatment was nearly a full grade point higher than her GPA from
the previous semester.
During the follow-up semester, Kimberly attended both booster sessions and five
mentoring sessions. She continued to have a strong relationship with her mentor and was eager to
meet with her. She stated that her transition to the new semester was easier than usual because
she was continuing to use the strategies she had learned from the program. She has made
considerable progress and views the program as a valuable support.
Discussion
The impaired functioning of college students with ADHD has critical implications for the
long-term financial and mental health status of this population, as well as for institutions of
higher learning concerned with graduation and retention rates, and for society as a whole.
Despite the obvious need for intervention, very little treatment research has been
conducted with this population to date (DuPaul & Weyandt, 2009; Green & Rabiner, 2012).
Although a well-controlled medication trial study recently has been published (DuPaul et al.,
2012), missing from the literature are studies investigating the efficacy of psychosocial
treatment. In response to this situation, our team has been developing and testing ACCESS, a
psychosocial treatment program for college students with ADHD.
Guided by conceptual considerations and empirical findings, ACCESS includes elements
of previously reported treatment protocols (Allsop et al., 2005; Prevatt et al., 2011; Safren et al.,
2005; Solanto, 2011) that have been blended together to create a developmentally appropriate
intervention that uses a unique combination of group CBT and individual mentoring to meet the
broad educational, psychological, social, and executive functioning needs of the ADHD college
population. Preliminary findings from this ongoing project are most encouraging. Attesting to the
construct validity of the design, there were clear improvements in the hypothesized mechanisms
of clinical change (i.e., ADHD knowledge, behavioral strategies, adaptive thinking), representing
large to very large effects. Medium to large effects were also associated with the significant
improvements observed in self-reported ADHD symptoms and executive functioning. Trends
approaching statistical significance further suggested that ACCESS may contribute to
improvements in emotional functioning. Also emerging from the data was preliminary evidence
of real-world educational benefits, along with increased utilization of campus resources.
This latter finding regarding campus resources warrants additional comment. ACCESS is
not intended to be a stand-alone intervention that addresses all of the challenges facing college
students with ADHD. On the contrary, ACCESS is designed to empower students with the
knowledge and skills necessary to better manage their ADHD and any comorbid conditions that
may be present, in part through the assistance it gives students in making connections with other
campus units that provide clinical services and other support. In this regard, ACCESS is best
viewed as an integral component of an overall multimodal treatment approach that includes other
interventions (e.g., medication management, counseling, tutoring).
Although promising, such findings are limited by the fact that ACCESS has thus far been
delivered in an open clinical trial. Future research must therefore include a control or comparison
group to determine whether these preliminary outcomes are in fact due to ACCESS versus
resulting from nonspecific therapeutic attention factors, the effects of repeated testing, and so on.
Another factor limiting any interpretation of these preliminary findings is the restricted range of
outcomes used in the design. To address this limitation, future research will need to
consider broadening the scope of outcomes in a way that includes not only multiple domains of
daily functioning but also less reliance on self-report. Because we have only analyzed a limited
amount of data from student records, we are not in a position to comment on the full impact of
ACCESS on educational functioning. Any statements on the stability of ACCESS-induced
improvements over time must also await our upcoming analyses of data collected from the
maintenance phase of our project.
Another unexplored area of great clinical interest is the degree to which a student’s level
of motivation and other individual differences predict successful outcome. Although most
students were actively engaged in ACCESS, some were not. Often, those not appropriately
engaged were freshmen whose parents had encouraged them to participate during their first
semester on campus. For others, dealing with comorbid depression or anxiety seemed to interfere
with their participation. For still others, holding down a job while attending school often led to
scheduling conflicts that made treatment adherence difficult. To determine for whom ACCESS is
best suited, it is critical that future research examine these and other individual differences.
To the extent that future research supports the preliminary findings from this study,
ACCESS can potentially serve as a model intervention for use on many college campuses. The
eight-week format that we now use for ACCESS would likely accommodate any variability in
the length of semesters, especially those ranging from 12 to 16 weeks. Such may not be the case,
however, for institutions using a quarterly rather than a semester system. There is also some
degree of flexibility in the setting in which ACCESS may be delivered. Given that most colleges
and universities have student counseling centers, this type of campus setting would seem
especially well suited to offering an ACCESS program. So too would an ODS, which is also
found on most campuses. Even more important than the convenience of the physical setting,
however, is the training and experience level of the staff housed within those settings. At a
minimum, successful implementation of ACCESS requires background and expertise in the use
of cognitive and behavioral therapy strategies. Advanced evidence-based knowledge of ADHD
as a disorder is also considered to be an important prerequisite for professionals delivering
ACCESS. Thus, campus staff that have these qualifications would likely be in a position to
deliver ACCESS effectively. Such an assumption, however, is yet untested and therefore will
need to be substantiated by future research.
In conclusion, ACCESS is a promising new psychosocial program that has great potential
for being used in many different college and university settings. Of even greater importance are
its potential public health benefits, in that ACCESS can serve as a protective factor that increases
the likelihood that students with ADHD can be more successful not only during college but also
as they begin their developmental transition into the postcollege adult world.
References
Allsop, D. H., Minskoff, E. H. & Bolt, L. (2005). Individualized course-specific strategy
instruction for college students with learning disabilities and ADHD: Lessons learned
from a model demonstration project. Learning Disabilities Research and Practice, 20,
103–118.
Barkley, R. A. (2006). Attention-deficit hyperactivity disorder: A handbook for diagnosis and
treatment (3rd ed.). New York, NY: Guilford Press.
Barkley, R. A., Murphy, K. R., DuPaul, G. J., & Bush, T. (2002). Driving in young adults with
attention deficit hyperactivity disorder: Knowledge, performance, adverse outcomes, and
the role of executive functioning. Journal of the International Neuropsychological
Society, 8, 655–672.
Barkley, R. A., Murphy, K. R., & Fischer, M. (2008). ADHD in adults: What the science says.
New York, NY: Guilford Press.
Beck, A., & Steer, T. (1993). Beck Anxiety Inventory. San Antonio, TX: Pearson Education.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory–II. San Antonio,
TX: Psychological Corporation.
Conners, C. K., Erhardt, D., & Sparrow, E. (2006). Conners’ Adult ADHD Rating Scales. Multi-
Health Systems.
DuPaul, G. J., Power, T. J., Anastopoulos, A. D., & Reid, R. (1998). Manual for the ADHD
Rating Scale–IV. New York, NY: Guilford Press.
DuPaul, G. J., Schaughency, E. A., Weyandt, L. L., Tripp, G., Kiesner, J., Ota, K., & Stanish, H.
(2001). Self-report of ADHD symptoms in university students: Cross-gender and cross-
national prevalence. Journal of Learning Disabilities, 34, 370–379.
DuPaul, G. J., & Weyandt, L. L. (2009). College students with ADHD: Current status and future
directions. Journal of Attention Disorders, 13, 234–250.
DuPaul, G. J., Weyandt, L. L., Rossi, J. S., Vilardo, B. A., O'Dell, S. M., Carson, K. M., . . .
Swentosky, A. (2012). Double-blind, placebo-controlled, crossover study of the efficacy
and safety of lisdexamfetamine dimesylate in college students with ADHD. Journal of
Attention Disorders, 16, 202–220.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (1996). Structured Clinical
Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV). Washington, DC:
American Psychiatric Press.
Fleming, A. P., & McMahon, R. J. (2012). Developmental context and treatment principles for
ADHD among college students. Clinical Child and Family Psychology Review, 15, 303–
329.
Gioia, G. A., Isquith, P. K., Guy, S., & Kenworthy, L. (2000). BRIEF: Behavior Rating
Inventory of Executive Function professional manual. Lutz, FL: Psychological
Assessment Resources.
Glutting, J. J., Youngstrom, E. A., & Watkins, M. W. (2005). ADHD and college students:
Exploratory and confirmatory factor structures with student and parent data.
Psychological Assessment, 17, 44–55.
Green, A. L., & Rabiner, D. L. (2012). What do we really know about college students with
ADHD? Neurotherapeutics, 9, 559–568.
Grenwald-Mayes, G. (2002). Relationship between current quality of life and family of origin
dynamics for college students with attention-deficit/hyperactivity disorder. Journal of
Attention Disorders, 5, 211–222.
Hecker, L., Burns, L., Elkind, J., Elkind, K., & Katz, L. (2002). Benefits of assistive reading
software for students with attention disorders. Annals of Dyslexia, 52, 243–272.
Heiligenstein, E., Guenther, G., Levy, A., Savino, F., & Fulwiler, J. (1999). Psychological and
academic functioning in college students with attention deficit hyperactivity disorder.
Journal of American College Health, 47, 181–185.
Heiligenstein, E., & Keeling, R. P. (1995). Presentation of unrecognized attention deficit
hyperactivity disorder in college students. Journal of American College Health, 43, 226–
228.
Kollins, S. H. (2008). ADHD, substance use disorders, and psychostimulant treatment: Current
literature and treatment guidelines. Journal of Attention Disorders, 12, 115–125.
Mannuzza, S., Gittelman-Klein, R., Bessler, A., Malloy, P., & LaPadula, M. (1993). Adult
outcome of hyperactive boys: Educational achievement, occupational rank, and
psychiatric status. Archives of General Psychiatry, 50, 565–576.
McKee, T. E. (2008). Comparison of a norm-based versus criterion-- based approach to
measuring ADHD symptomtology in college students. Journal of Attention Disorders, 11,
677–688.
Meaux, J. B., Green, A., & Broussard, L. (2009). ADHD in the college student: A block in the
road. Journal of Psychiatric and Mental Health Nursing, 16, 248–256.
Norvilitis, J. M., Ingersoll, T., Zhang, J., & Jia, S. (2008). Self-reported symptoms of ADHD
among college students in China and the United States. Journal of Attention Disorders,
11, 558–567.
Norwalk, K., Norvilitis, J. M., & MacLean, M. G. (2008). ADHD symptomatology and its
relationship to factors associated with college adjustment. Journal of Attention Disorders,
1–8.
Prevatt, F., Lampropoulos, G. K., Bowles, V., & Garrett, L. (2011). The use of between session
assignments in ADHD coaching with college students. Journal of Attention Disorders,
15, 18–27.
Pryor, J. H., Hurtado, S., DeAngelo, L., Blake, L. P., & Tran, S. (2010). The American
freshman: National norms fall 2010. Los Angeles, CA: Higher Education Research
Institute, University of California, Los Angeles.
Rabiner, D. L., Anastopoulos, A. D., Costello, J., Hoyle, R. H., & Swartzwelder, H. S. (2008).
Adjustment to college in students with ADHD. Journal of Attention Disorders, 11, 689–
699.
Reaser, A., Prevatt, F., Petscher, Y., & Proctor, B. (2007). The learning and study strategies of
college students with ADHD. Psychology in the Schools, 44, 627–638.
Richards, T. L., Deffenbacher, J. L., & Rosén, L. A. (2002). Driving anger and other driving-
related behaviors in high and low ADHD symptom college students. Journal of Attention
Disorders, 6, 25–38.
Safren, S. A., Perlman, C. A., Sprich, S., & Otto, W. (2005). Mastering your adult ADHD: A
cognitive-behavioral treatment program therapist guide. New York, NY: Oxford
University Press.
Shaw-Zirt, B., Popali-Lehane, L., Chaplin, W., & Bergman, A. (2005). Adjustment, social skills,
and self-esteem in college students with symptoms of ADHD. Journal of Attention
Disorders, 8, 109–120.
Solanto, M. V. (2011). Cognitive-behavioral therapy for adult ADHD: Targeting executive
dysfunction. New York, NY: Guilford Press.
Upadhyaya, H. P., Rose, K., Wang, W., O’Rourke, K., Sullivan, B., Deas, D., & Brady, K. T.
(2005). Attention-deficit/hyperactivity disorder, medication treatment, and substance use
patterns among adolescents and young adults. Journal of Child and Adolescent
Psychopharmacology, 15, 799–809.
Weyandt, L. L., Iwaszuk, W., Fulton, K., Ollerton, M., Beatty, N., Fouts, H., . . . Greenlaw, C.
(2003). The internal restlessness scale: Performance of college students with and without
ADHD. Journal of Learning Disabilities, 36, 382–389.
Wolf, L. E. (2001). College students with ADHD and other hidden disabilities: Outcomes and
interventions. In J. Wasserstein, L. E. Wolf, & F. F. LeFever (Eds.), Adult attention
deficit disorder: Brain mechanisms and life outcomes (pp. 385–395). New York, NY:
New York Academy of Sciences.
